 WHAT IS THE DIFFERENCE BETWEEN TELEHEALTH, TELEMEDICINE & REMOTE MONITORING?
WHAT IS THE DIFFERENCE BETWEEN TELEHEALTH, TELEMEDICINE & REMOTE MONITORING?
In general:
- Telehealth refers to a broader scope using of electronic information and telecommunications technologies to support distance clinical health care, patient and professional health-related education, public health and health administration. For example, telehealth includes clinician to clinician consults, patient education services, interprofessional care team communications, and more! Some other terms for telehealth include "Connected Care" and "Digital Health".
- Telemedicine typically refers to remote clinical services between a provider and a patient/client where a physician/clinician in one location uses a telecommunications infrastructure to deliver care to a patient at a distant site. Telemedicine is a subset of telehealth.
- Remote patient monitoring refers to using technology to gather patient data outside of traditional healthcare settings, for example, using digital scales, glucometers, pulse ox devices, etc…to monitor a patient’s condition while they are at home (or wherever else they may be living). It too is a subset of telehealth.
- So where does mHealth fit in? mHealth is an abbreviation for mobile health. It simply refers to the subset of telehealth that use mobile technologies. Examples include apps and peripheral devices designed for use on smart phones and tablets for videoconferencing or gathering patient data or providing patient education or secure communications.
 GETTING STARTED
GETTING STARTED
Getting Started with Telehealth
- How can telehealth be used in response to COVID-19?
- For a high level overview of how telehealth can be used in response to COVID-19 in a variety of settings (public health, facilities and practices, and more) take a look at these resources:
- COVID-19 Telehealth Toolkit:
- Conceptual framework for telemedicine for COVID-19
- New England Journal of Medicine article on COVID-19 and Health Care's Digital Revolution
- Tip Sheet: Application of Telemedicine and Telecritical Care to Emergency Management of COVID-19
- Digital Health and the Fight Against the COVID-19 Pandemic
- Pandemic Response Technology Response Plan examines eleven critical areas of need for healthcare delivery when responding to the COVID-19 pandemic and see all the ways in which technology technologies offer a solution.
- For a high level overview of how telehealth can be used in response to COVID-19 in a variety of settings (public health, facilities and practices, and more) take a look at these resources:
-
- Of particular interest to how telehealth can be used in response to COVID-19 for those who work in clinical practice (both inpatient and outpatient) settings, take a look at these resources:
- Electronic Personal Protective Equipment: A Strategy to Protect Emergency Department Providers in the Age of COVID-19
- Use of E-Consults for reducing exposure:
- E-Consult toolkit
- Webinar on Inpatient eConsults
- Of particular interest to how telehealth can be used in response to COVID-19 for those who work in clinical practice (both inpatient and outpatient) settings, take a look at these resources:
-
-
-
- Free self paced online training module with 1 CME/CE credit on The Use of Telehealth for eConsultation (eConsults)
- Free self paced online training module with 1 CME/CE credit on creating a telehealth enabled Isolation Communication Management System (iSOCOMS) to care for patients hospitalized with a highly infectious pathogen.
-
-
- What do I need to think about before I get started with telehealth?
- If time is of the essence, and you are looking to make a rapid pivot, check out these resources:
- This approximately 45 minute video will help walk you through the high level essentials you’ll need to think through as you get started:
- If time is of the essence, and you are looking to make a rapid pivot, check out these resources:
If you don't have time for the video, or want something in paper format after watching the video, download this companion infographic: Telehealth Essentials Checklist: For Those Getting Started.
-
-
- Take a look at this Quick-Start Guide to Telehealth During a Health Crisis developed by the American Telemedicine Association.
-
-
-
- Explore the Telehealth Basics section of the National Consortium of Telehealth Resource Centers website.
-
-
- If you have some time, check out these training opportunities and implementation toolkits:
- You can receive 1 credit/contact hour of CME/CE credits for taking this online self-paced Foundations of Telehealth Course Module. There is a $59 fee associated with this course.
- Another alternative is this American College of Physicians course that also offers CME credits called Telemedicine: A Practical Guide for Incorporation into your Practice.
- A third alternative is the American Medical Association STEPS Forward module on Telemedicine: Facilitate Access to Care for Your Patients that also offers CME credits.
- If you or others in your practice will be providing any kind of logistical/administrative support for telehealth visits, this is a great training (FREE, but registration required) Telehealth Coordinator Online Training.
- California TRC Telehealth Program Developer Kit
- AHIMA Telemedicine Toolkit
- HHS Telehealth Resources for Health Care Providers
- If you have some time, check out these training opportunities and implementation toolkits:
- Now that I have the high level basics, what next?
- Work your way through the rest of the information in this COVID-19 Toolkit! We strongly recommend that you get familiar with all sections in this toolkit, but if time is of the essence, then proceed to the section on Best Practices for Conducting a Telehealth Visit as this will help you think about workflow, consent, documentation and more. You may also want to check out our Resources for Specialty Providers and Settings where we have specialized resources for dentists, genetics counselors, hospice and palliative care providers, rehabilitation professionals and more!
-
- After reviewing all of the resources and information found here, if you have additional questions, join us for our Virtual Office Hours where you can ask questions, bounce ideas and more.
-
- You may also Request Technical Assistance using our online form
- To see a list of a variety of training resources, visit this Telehealth Course Finder and visit the Telehealth Village Course Catalog.
(Hot Tip: Due to the overwhelming interest and need for telehealth during this pandemic, using the online form will generally get you a quicker response than calling and leaving a voicemail message. It is much more difficult to return calls after hours and on weekends, but we CAN respond to your emails. The more specific you are with your question or request (e.g., what type of provider you are, what type of setting you work in, what you specifically need), the better we will be at getting you timely and useful information.)
Getting Started with Telemental/Behavioral Health
- How can telehealth be used by mental/behavioral health clinicians and practices?
- Check out this brief one minute introductory video taken from our Telebehavioral Health Center of Excellence website:
- What do I need to think about before I get started with telemental/behavioral health?
-
- View our training on Telebehavioral Health 101: This session provides a high-level overview of basic definitions, benefits and evidence base, use cases, applicable technologies, professional ethics, and business models. This session will also take a high level look at key federal and state policy and reimbursement considerations, including the potential implications of changes that have taken place due to COVID-19..
-
- View our training on Telebehavioral Health 201: This session guides you through best practices for setting up and starting a HIPAA-compliant Telemental Health or Telebehavioral Health service in an agency, hospital or private practice setting. Topics covered will include identifying HIPAA-secure software, handling emergencies, creating referral relationships, integrating services into your current practice, getting informed consent and more.
-
- If you are serious about telemental/behavioral health, you can get yourself Board Certified as a Telemental Health Provider through the National Board for Certified Counselors. You may access the modules through New College Institute StarTelehealth. There are a total of 9 modules at $50 per module or $400 for the whole series).
-
- For other course/training resources with certificates or CME/CEs:
- Visit the Telehealth Certification Institute
- Check out this free online course developed by Array on Telebehavioral Health Best Practices
- Visit the Telehealth Course Finder.
- For other course/training resources with certificates or CME/CEs:
-
- If you are a psychiatrist, here are some training opportunities specific to Telepsychiatry:
- Visit Telehealth Village for the Telemental Health - Introductory Module Telepsychiatry ($79 to take the module and includes CME/CE)
- Check out this free webinar on Telepsychiatry in the Era of COVID-19 developed in conjunction with the American Psychiatric Association and the Substance Abuse and Mental Health Services Administration (SAMHSA).
- If you are a psychiatrist, here are some training opportunities specific to Telepsychiatry:
- Now that I have the high level basics, what next?
- Visit the Clinical Guidelines section of our Telebehavioral Center of Excellence Website to start with, and then go on to explore the other sections! You'll find that we have curated many resources. Here are a few of the types of things you will find:
- The American Telemedicine Association in partnership with the American Psychiatric Association has put together Best Practices in Videoconferencing-Based Telemental Health (April 2018)
- The American Telemedicine Association has developed Practice Guidelines for Telemental Health with Children and Adolescents.
- The American Psychological Association has developed the following resources:
- The American Psychiatric Association has developed the following toolkits:
- The Inter Organizational Practice Committee (IOPC) has put together this Tele-Neuropsychology Toolkit that includes practice recommendations and guidelines, models, trainings and webinars and more.
- HHS has put together this Best Practice Guide: Telehealth for Behavioral Health Care
- If you do any kind of psychological assessments or testing, here are a few resources for you
- Visit the Clinical Guidelines section of our Telebehavioral Center of Excellence Website to start with, and then go on to explore the other sections! You'll find that we have curated many resources. Here are a few of the types of things you will find:
- What if I have patients/clients with specific clinical issues/needs?
-
- The Mental Health Technology Transfer Center Network funded by SAMHSA has a Clinical Innovations in Telehealth Learning Series, Sessions were recorded and posted online. Session topics include things like Telehealth and Suicide Care, Telehealth and CBTp for Psychosis, Providing Culturally Relevant Telehealth Services, and Treating PTSD.
-
- How should I manage a suicidal patient/client?
- Here is a learning session on Telehealth and Suicide Care:
-
- The Center for Practice Innovation has developed Telehealth Tips: Managing Suicidal Clients During the COVID-19 Pandemic. The document includes a Patient Safety Plan Template for you to use.
-
- This International Journal of Psychiatry in Medicine publication on Suicide Risk Management During Clinical Telepractice provides information about safety protocols and suicide risk assessment procedures used with U.S. military service members and veterans with depression.
- How should I manage victims of intimate partner/domestic violence or abuse?
- CASA is encouraging telehealth professionals to develop a code word to use when working with survivors to indicate if a perpetrator is in the room or within earshot. You would need to have done this in advance or during a time when you know for certain that the perpetrator is not around. For example, if you have met with a client and pre-arranged a code word (e.g., Walmart), and you notice a behavior change (or consider doing this at the start of every session), you could say following:
You: Have you gone to Walmart today?
Client: Yes (perpetrator is present), No (all clear)
You: Did you find what you needed?
Client: Yes (everything is fine and I am safe), No (please call 911 I am unsafe)
If they say yes then continue with your check in but do not go much deeper (e.g, avoid discussion of safety plans etc) so that you don’t tip the perpetrator off that you know they are there. In addition, if a Client brings up a statement about Walmart such as “I need to go to Walmart today”, it is an indicator that the perpetrator has walked in or is close by so you can begin to wrap things up.
-
- The National Network to End Domestic Violence has developed a number of resources:
- Using Technology to Communicate with Survivors During a Public Health Crisis, which also includes links to their Digital Services Toolkit on best practices for using tools such as text, chat and video
- The National Network to End Domestic Violence has developed a number of resources:
-
-
- Here is a video on COVID-19 & Survivor Confidentiality:
-
- How do I care for clients/patients who are in inpatient, residential or other non-ambulatory care settings?
- The American Psychiatric Association and the National Association for Behavioral Healthcare jointly hosted a recorded discussion with experts on How to Address COVID-19 Across Inpatient, Residential and Other Non-ambulatory Care Settings. The recording is available for free and CMEs are available (registration required).
- How do I care for clients/patients with serious mental illness?
- Here is a learning session on Telehealth and Cognitive Behavioral Therapy for Psychosis (CBTp):
-
- The American Psychiatric Association and the National Association for Behavioral Healthcare jointly hosted a recorded discussion with experts on Serious Mental Illness and COVID-19: Tailoring ACT Teams, Group Homes and Supportive Housing. The recording is available for free (registration required).
-
- Array is offering this online 1 CME credit training course on Treating Serious Mental Illness via Telepsychiatry free of charge during the pandemic.
-
- The Substance Abuse and Mental Health Services Administration (SAMHSA) as part of their Evidence-Based Resource Guide Series has developed Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders
- Are there any special considerations for working with rural populations, particularly the elderly?
- Array is offering this online 1 CME credit training course on Telepsychiatry for Rural Elderly free of charge during the pandemic.
(Hot Tip: Due to the overwhelming interest and need for telehealth during this pandemic, using the online form will generally get you a quicker response than calling and leaving a voicemail message. It is much more difficult to return calls after hours and on weekends, but we CAN respond to your emails. The more specific you are with your question or request (e.g., what type of provider you are, what type of setting you work in, what you specifically need), the better we will be at getting you timely and useful information.)
Getting Started with Remote Patient Monitoring
- Help me understand remote patient monitoring?
- Check out this brief under a minute introductory video taken from our Remote Patient Monitoring Toolkit on our website. This toolkit is dedicated to helping providers get started. Visit the toolkit and make sure you download the actual RPM Toolkit (it's an 8 page PDF document with lots of great information).
- What are some use cases for remote patient monitoring? There are many ways the remote patient monitoring is being used. Here are a few examples:
- The American Heart Association has issued Using Remote Patient Monitoring Technologies for Better Cardiovascular Disease Outcomes Guidance
- The Personal Connected Health Alliance has put together this article on Understanding Remote Patient Monitoring in COPD
- The Rural Health Information Hub has this spotlight on Telehealth Invigorating and Innovating Diabetes Care
- mHealth Intelligence published an article on Telehealth Gives Patients a Real-Time Link to Mental Health Support
- The California Health Care Foundation published this paper on Remote Patient Monitoring in the Safety Net: What Payers and Providers Need to Know
- What kinds of devices can be used for remote patient monitoring?
- The US Food & Drug Administration (FDA) has issued a new policy that allows manufacturers of certain FDA-cleared non-invasive vial sign-measuring devices to expand their use so that health care providers can use them to monitor patients remotely. The devices include those that measure body temperature, respiratory rate, heart rate and blood pressure.
 NAVIGATING HIPAA, BROADBAND, TECHNOLOGY AND VENDORS
NAVIGATING HIPAA, BROADBAND, TECHNOLOGY AND VENDORS
Digital Health Literacy, Device Equity and Broadband Access Resources
- Telehealth Access for Seniors provides seniors and low-income communities with devices, instructions and free tech-support to connect them to their physicians via telehealth through the generosity of donations and volunteers. Visit their website to donate, request technical support (individuals) or to request assistance with accessing phones/tablets for your patients (clinics only).
- The National Digital Equity Center advocates for Digital Inclusion which includes Affordable Broadband, Affordable Equipment and Public Computer Access. The National Digital Equity Center is focused on creating digitally literate citizens across Maine and beyond, providing communities with the expertise to mobilize broadband technologies through digital inclusion and literacy efforts. While many of the resources are focused on Maine, there are also many educational resources applicable to all including online webinars/classes.
- COVID Tech Connect was founded with a mission to connect critically ill COVID-19 patients with their loved ones by donating smart devices to hospitals and care facilities across the country. They are currently offering 5-15 devices per facility, giving priority to those in greatest need.
- iCanConnect, also known as the National Deaf-Blind Equipment Distribution Program (NDBEDP), was established by the Federal Communications Commission (FCC). iCanConnect provides free equipment including smartphones, tablets, computers, screen readers, braille displays, and more to people who meet federal disability and income guidelines.
- National Assistive Technology Act Technical Assistance and Training (AT3) Center is your one-stop connection to information about the Assistive Technology Act, State Assistive Technology Programs, and general assistive technology and has this Program Directory of State Assistive Technology Programs.
- Telehealth Equity Coalition is building a wide coalition of supporters to advocate for greater access to telehealth, with a specific focus on broadband and hardware access, digital and health literacy, trust and accountability, social determinants of health, educating communities about telehealth and evidence and value based care.
- Digitunity (Digital Opportunity Network) is working to eliminate the technology gap in partnership with a network of stakeholders. While not focused on health care, some of their initiatives include refurbishing computers and creating pathways to device ownership.
- Cellular/Wireless Service: All four of the major United States carriers have signed on to the FCC’s Keep Americans Connected Pledge. Under this agreement, carriers have agreed to take the follow action for at least the next 60 days: 1) Not terminate service to any residential or small business customers because of their inability to pay their bills due to the disruptions caused by the coronavirus pandemic; 2) Waive any late fees that any residential or small business customers incur because of their economic circumstances related to the coronavirus pandemic; and 3) Open its Wi-Fi hotspots to any American who needs them.
- AT&T is currently offering home internet wireline customers unlimited data. New customers who are eligible for public assistance programs can subscribe to Access from AT&T for two months of free service. All public WiFi hotspots are open to anyone who needs them. AT&T will not terminate service of any wireless, phone or broadband residential or small business customer due to an inability to pay your bill. All late payment fees will be waived.
- Verizon will not charge late fees or terminate service to customers who are experiencing hardships because of COVID-19 and cannot pay their bill in full.
- Sprint is providing unlimited data for 60 days to customers with metered data plans effective 3/18/20.
- T-Mobile is providing customers on smartphone plans unlimited data for 60 days effective 3/13/20. Customers should dial 611 on their T-Mobile phone if they have concerns about bill payments due to COVID-19.
- Internet Service: In response to the coronavirus pandemic and its impact on society, multiple Internet Service Providers (ISPs) have made updates to their low-cost internet service programs to ensure individuals and families stay connected to the internet.
- To find low-cost Internet Service and Computers in Your Area, use this tool from everyoneon!
- The Affordable Connectivity Program: Helps low-income households pay for internet service and connected devices. If your household is eligible, you can receive: 1) up to $30/month discount on your internet service; 2) up toe a $75/month discount if your household is on qualifying Tribal lands and 3) a one-time discount of up to $100 for a laptop, tablet or desktop computer (with a co-payment of more than $10 but less than $50). A household is eligible if:
- Your household income is 200% or less than the Federal Poverty Guidelines.
- You participate in certain government assistance programs, such as SNAP, Medicaid, WIC, SSI, FPHA, Veterans Pension and Survivors Benefits, Free and Reduced-Price School Lunch Program or School Breakfast Program or received a Federal Pell Grant in the current award year.
- You live on qualifying Tribal lands of if someone in your household participates in Bureau of Indian Affairs General Assistance; Head Start; Tribal TANF or Food Distribution Programs on Indian Reservations.
- You already receive a Lifeline Benefit.
- If your child or dependent participates in the Free and Reduced-Price School Lunch Program or is enrolled in a USDA Community Eligibility Provision school.
-
- It was recently brought to our attention that the Halo Cellular Gateway might be a budget friendly (relatively speaking) way to bring broadband to areas with limited or no broadband access.
- Other Creative Solutions: While helping those who can't afford broadband to access it is useful if there is cellular or cable of fiber solution, there still remain areas in the U.S. that simply do not have this infrastructure. Some creative ways to help people access the internet that have been used include:
- Making available wi-fi access from schools, libraries, and other business parking lots so that individuals can access the wi-fi from their cars or even retro-fitting library study rooms or un-used spaces in schools to provide private spaces.
- Developing public wi-fi access points in the community such as in an abandoned store fronts or other un-used community facilities.
- Putting in kiosks with devices in areas of the community that do have broadband access.
- Check out this example from the Delaware Libraries: https://technical.ly/delaware/2021/05/11/delaware-libraries-telehealth-kiosks/ They are using this for their kiosk: https://www.talkboxbooth.com/. For those who want more information about the library initiative, here are two webinars:
Telehealth and HIPAA
- Give me the quick and dirty basics about HIPAA and Telehealth
- For a quick introduction to HIPAA Compliance and Telehealth, watch this brief video:
-
- You might also want to check out this HIPAA & Telehealth Infographic
- Is it true that I don't have to worry about HIPAA during the pandemic? Since most of you are frantically trying to get started yesterday, if you don't currently have any technology that you could use for a telehealth visit, please know that as part of its response to the pandemic, a change was made regarding HIPAA. The HHS Office for Civil Rights (OCR) is exercising enforcement discretion and waiving penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype. See FAQs on Telehealth and HIPAA during the COVID-19 Nationwide Public Health Emergency.
The intent of the OCR response to the pandemic is for providers to act responsibly and to make every effort to comply ("in good faith") with HIPAA in terms of technology selection and communications channels. This is particularly important when working with patients who might have sensitive health information. If you are using everyday communications technologies without encryption on a public wi-fi network, this is extra risky and you need to seriously weigh the risks against the benefits. If the situation is urgent/emergent, and you don't have other methods, by all means. However, if the situation is less urgent and you can arrange for a platform with encryption and/or move to a more private setting, you would be strongly advised to do so. With that said, please check your State policies, as not every state has waived enforcement of their HIPAA requirements.
-
- To check your State policies, Click Here, select the state of interest and then scroll down to the lower half of the page to see the original guidance documents and any new guidance related to COVID-19. Alternatively, just go up to the top menu bar and select your state under "Our Region".
-
- If you are considering using everyday communications technologies during this pandemic, the Health Information Technology Evaluation and Quality Center (HITEQ) has put together a very nice Issue Brief on Using non-traditional technology for telehealth during COVID-19 Pandemic that would be worth your time to review.
- What's all this news about Zoom-Bombing and what is the risk to privacy and security? While the "free" version of Zoom is not recommended for telehealth visits (there is a paid health care version that has more of the elements required by HIPAA), we know many of you are using it as a stopgap measure or for administrative meetings. In order to make Zoom user friendly, Zoom had set its "default" settings to be as open as possible. The majority of the issues you've heard/read about in the media were related to users not bothering to make adjustments to these default settings. This article on How to Prevent Zoom-Bombing provides some very practical information on how to mitigate the majority of the risks. Since this time, Zoom has updated their platform several times, changing many of the problematic default settings to more secure default settings.
- Are there any privacy/security issues related to using bluetooth headphones or other bluetooth devices for telehealth? Bluetooth can be a privacy/security risk. Bluetooth is an open standard for short-range radio frequency communication. If your mobile device has Bluetooth capability, turn off or set the Bluetooth connection capabilities to “nondiscoverable.” When in discoverable mode, Bluetooth-enabled mobile devices are “visible” to other nearby devices, which may alert a hacker to target them. When Bluetooth is turned off or in nondiscoverable mode, the Bluetooth-enabled mobile devices are invisible to other devices not authorized to access or monitor the data in your device. It is definitely not advisable to use Bluetooth in a public place or with a public network. Additionally, as with passwords, you should never share your Bluetooth pairing codes with anyone. For more information, take a look at this NIST Guide to Bluetooth Security.
- What do I need to know about HIPAA and audio only/telephone visits? The FCC issued a Declaratory Ruling and Order to clarify HIPAA rules and how they apply to telephone calls with patients. A very good summary of the rule may be found here. The enforcement discretion and waiver of penalties granted by OCR in response to the pandemic also applies to landline and wireless communications.
- I am trying to prepare for telehealth post-pandemic. What do I need to know about HIPAA and Telehealth? Here are several resources that can be used to help you prepare to do your own risk assessment:
- HIPAA Compliance Roadmap (Created by Behavioral Health Innovation)
- Telehealth Compliance Checklist (Created by Foley & Lardner, LLP)
- Telehealth Audit Checklist (Created by eCatalyst)
Working with Vendors (Technology and Service Providers)
- How do I got about selecting a vendor for telehealth technology or services? If you have a budget for technology and infrastructure and the luxury of taking a little time, we would recommend your using our Vendor Selection Toolkit.to better help you determine your technology and/or clinical requirements before selecting a vendor(s).
- There are so many technologies out there. How do I figure out what will meet my clinical requirements?
- The National Telehealth Technology Assessment Resource Center (TTAC) has put together a number of Toolkits to assist you with learning the fundamentals of the various technologies and how to assess those technologies. They have also created an Innovation Watch section that takes a closer look at new technologies as they come to market.
- Available Toolkits (includes a Clinician's Guide to Video Platforms)
- Innovation Watch
- The National Telehealth Technology Assessment Resource Center (TTAC) has put together a number of Toolkits to assist you with learning the fundamentals of the various technologies and how to assess those technologies. They have also created an Innovation Watch section that takes a closer look at new technologies as they come to market.
- How do I know what types of vendors are out there? If you are exploring what types of vendors are out there:
-
- If you are looking for telehealth service providers, the Southwest Telehealth Resource Center has put together this Service Provider Directory for Telemedicine and Telehealth.
- If you are looking for telehealth companies, Becker's Hospital Review has put together this list of 260+ Telehealth Companies to Know
Free/Low Cost Telehealth Technology Solutions and Services
Critical Care: The National Emergency Tele-Critical Care Network is a joint program of the U.S. Department of Health & Human Services (HHS) and the U.S. Department of Defense (DoD). It is available at no cost to hospitals caring for COVID-19 patients and struggling with access to enough critical care physicians, nurses, respiratory therapists, and other specialized clinical experts. Teams of critical care clinicians are available to deliver virtual care through telemedicine platforms, such as an app on a mobile device. Hear from participating clinicians, and click here to request assistance. Communications
- Significantly reduced pricing on Updox Secure Text for 6 months.
- Free Presence Scheduling and Telemedicine Solution
- Instant Language Assistant (Medical) software/app temporarily available to providers free during the pandemic.
- Free sign language Virtual Remote Interpretation by linguabee for COVID-19 test sites
- Free access to Safety Net Connect eConsult Telehealth Portal for primary care physicians
- Free access to ConferMED Coronavirus eConsults for Safety Net Practices
- Free access to The MAVEN Project for eConsults for community health clinics who serve the underserved.
- Free access to RubiconMD for 120+ specialties for qualifying safety net clinicians. Clinic leadership should contact covid19support@rubiconmd.com
- AireHealth Portable Nebulizer Kit on sale at significantly reduced rate with additional $25 off first nebulizer kit and free shipping with code WELCOME25
- Eko Telehealth is giving health systems 30 days of complimentary access to their stethoscope live streaming software and cardiac screening AI platform.
- Free access to Vivovitals remote patient monitoring platform for providers in the United States
- Significantly reduced pricing on Connected Healthcare Solutions (CHS) Health Guidance Platform for remote monitoring (reduced one time startup fee with no minimum quantities or contractual requirements - and use as many or as few devices as you need with no additional cost)
- LSI Rentals and Leasing Options offers both short and longer term rental and leasing options for patient monitoring equipment
- Free 90 day trial of KangarooHealth intelligent remote patient monitoring platform by contacting Bridget Holm
- Free use of Orbita COVID-19 Screening Chatbot & Knowledge Base through June 2020
- Hospitals can add for free Bright.md's coronavirus screening tool, based on its asynchronous virtual care delivery platform, SmartExam, to their websites. The online tool guides patients through a dynamically adaptive online medical interview, reviewing their symptoms and health history, as well as possible exposure to COVID-19.
- findhelp has a search platform that is free and open to help locate free and reduced-cost program resources to meet social need.
- Unite Us has a digital technology platform that connects organizations to each other to track referrals and outcomes. Community network partners (e.g., housing services, food assistance, behavioral health etc) can join for free.
- Free trial of Vyopta Platform for automating compliance reporting and system utilization and capacity monitoring for hospitals and health systems scaling up to 1K end users or more.
- Free 60 day trial access to Bluestream virtual care platform
- Free temporary access to Compunetix Video Call Center for Healthcare platform with no fees or obligations
- Free white-labeled RingMD telemedicine platform for doctors, healthcare groups and other organizations negatively affected by the outbreak.
- Free Cloudbreak Health unified telemedicine and video medical interpretation solution app with free service for hospitals
- Free Allm JOIN platform in the ED and JOIN Triage to EMS/ambulance providers to facilitate quick assessment, routing to appropriate hospital, pre-notification to destination hospital, bi-directional communication including video calls. Works in conjunction with radio and other existing systems.
- Free basic and significantly reduced pricing on full featured Adaptive Telehealth telemental health platform license
- Free standard plan (supported by promotions and advertising) through Vivadox
- Free basic doxy.me telemedicine platform
- Free basic doximity temedicine platform
- Free TeleHome video call platform designed for to help caregivers connected isolated COVID-19 patients with loved ones on any device, anywhere.
- $3 pay per use plan (other plans available) and free imaging with Nautilus Medical Technologies teleray video & audio communication and dicom image exchange solution.
- Free trial access to CompuGroup Medical US CGM ELVI web-based video platform
- Free Pulsara ONE + COVID-1g video-enabled platform to all EMS and healthcare organizations
- Significantly reduced pricing on Updox Video Chat for 6 months.
In general:
- Telehealth refers to a broader scope using of electronic information and telecommunications technologies to support distance clinical health care, patient and professional health-related education, public health and health administration. For example, telehealth includes clinician to clinician consults, patient education services, interprofessional care team communications, and more! Some other terms for telehealth include "Connected Care" and "Digital Health".
- Telemedicine typically refers to remote clinical services between a provider and a patient/client where a physician/clinician in one location uses a telecommunications infrastructure to deliver care to a patient at a distant site. Telemedicine is a subset of telehealth.
- Remote patient monitoring refers to using technology to gather patient data outside of traditional healthcare settings, for example, using digital scales, glucometers, pulse ox devices, etc…to monitor a patient’s condition while they are at home (or wherever else they may be living). It too is a subset of telehealth.
- So where does mHealth fit in? mHealth is an abbreviation for mobile health. It simply refers to the subset of telehealth that use mobile technologies. Examples include apps and peripheral devices designed for use on smart phones and tablets for videoconferencing or gathering patient data or providing patient education or secure communications.
Getting Started with Telehealth
- How can telehealth be used in response to COVID-19?
- For a high level overview of how telehealth can be used in response to COVID-19 in a variety of settings (public health, facilities and practices, and more) take a look at these resources:
- COVID-19 Telehealth Toolkit:
- Conceptual framework for telemedicine for COVID-19
- New England Journal of Medicine article on COVID-19 and Health Care's Digital Revolution
- Tip Sheet: Application of Telemedicine and Telecritical Care to Emergency Management of COVID-19
- Digital Health and the Fight Against the COVID-19 Pandemic
- Pandemic Response Technology Response Plan examines eleven critical areas of need for healthcare delivery when responding to the COVID-19 pandemic and see all the ways in which technology technologies offer a solution.
- For a high level overview of how telehealth can be used in response to COVID-19 in a variety of settings (public health, facilities and practices, and more) take a look at these resources:
-
- Of particular interest to how telehealth can be used in response to COVID-19 for those who work in clinical practice (both inpatient and outpatient) settings, take a look at these resources:
- Electronic Personal Protective Equipment: A Strategy to Protect Emergency Department Providers in the Age of COVID-19
- Use of E-Consults for reducing exposure:
- E-Consult toolkit
- Webinar on Inpatient eConsults
- Of particular interest to how telehealth can be used in response to COVID-19 for those who work in clinical practice (both inpatient and outpatient) settings, take a look at these resources:
-
-
-
- Free self paced online training module with 1 CME/CE credit on The Use of Telehealth for eConsultation (eConsults)
- Free self paced online training module with 1 CME/CE credit on creating a telehealth enabled Isolation Communication Management System (iSOCOMS) to care for patients hospitalized with a highly infectious pathogen.
-
-
- What do I need to think about before I get started with telehealth?
- If time is of the essence, and you are looking to make a rapid pivot, check out these resources:
- This approximately 45 minute video will help walk you through the high level essentials you’ll need to think through as you get started:
- If time is of the essence, and you are looking to make a rapid pivot, check out these resources:
If you don't have time for the video, or want something in paper format after watching the video, download this companion infographic: Telehealth Essentials Checklist: For Those Getting Started.
-
-
- Take a look at this Quick-Start Guide to Telehealth During a Health Crisis developed by the American Telemedicine Association.
-
-
-
- Explore the Telehealth Basics section of the National Consortium of Telehealth Resource Centers website.
-
-
- If you have some time, check out these training opportunities and implementation toolkits:
- You can receive 1 credit/contact hour of CME/CE credits for taking this online self-paced Foundations of Telehealth Course Module. There is a $59 fee associated with this course.
- Another alternative is this American College of Physicians course that also offers CME credits called Telemedicine: A Practical Guide for Incorporation into your Practice.
- A third alternative is the American Medical Association STEPS Forward module on Telemedicine: Facilitate Access to Care for Your Patients that also offers CME credits.
- If you or others in your practice will be providing any kind of logistical/administrative support for telehealth visits, this is a great training (FREE, but registration required) Telehealth Coordinator Online Training.
- California TRC Telehealth Program Developer Kit
- AHIMA Telemedicine Toolkit
- HHS Telehealth Resources for Health Care Providers
- If you have some time, check out these training opportunities and implementation toolkits:
- Now that I have the high level basics, what next?
- Work your way through the rest of the information in this COVID-19 Toolkit! We strongly recommend that you get familiar with all sections in this toolkit, but if time is of the essence, then proceed to the section on Best Practices for Conducting a Telehealth Visit as this will help you think about workflow, consent, documentation and more. You may also want to check out our Resources for Specialty Providers and Settings where we have specialized resources for dentists, genetics counselors, hospice and palliative care providers, rehabilitation professionals and more!
-
- After reviewing all of the resources and information found here, if you have additional questions, join us for our Virtual Office Hours where you can ask questions, bounce ideas and more.
-
- You may also Request Technical Assistance using our online form
- To see a list of a variety of training resources, visit this Telehealth Course Finder and visit the Telehealth Village Course Catalog.
(Hot Tip: Due to the overwhelming interest and need for telehealth during this pandemic, using the online form will generally get you a quicker response than calling and leaving a voicemail message. It is much more difficult to return calls after hours and on weekends, but we CAN respond to your emails. The more specific you are with your question or request (e.g., what type of provider you are, what type of setting you work in, what you specifically need), the better we will be at getting you timely and useful information.)
Getting Started with Telemental/Behavioral Health
- How can telehealth be used by mental/behavioral health clinicians and practices?
- Check out this brief one minute introductory video taken from our Telebehavioral Health Center of Excellence website:
- What do I need to think about before I get started with telemental/behavioral health?
-
- View our training on Telebehavioral Health 101: This session provides a high-level overview of basic definitions, benefits and evidence base, use cases, applicable technologies, professional ethics, and business models. This session will also take a high level look at key federal and state policy and reimbursement considerations, including the potential implications of changes that have taken place due to COVID-19..
-
- View our training on Telebehavioral Health 201: This session guides you through best practices for setting up and starting a HIPAA-compliant Telemental Health or Telebehavioral Health service in an agency, hospital or private practice setting. Topics covered will include identifying HIPAA-secure software, handling emergencies, creating referral relationships, integrating services into your current practice, getting informed consent and more.
-
- If you are serious about telemental/behavioral health, you can get yourself Board Certified as a Telemental Health Provider through the National Board for Certified Counselors. You may access the modules through New College Institute StarTelehealth. There are a total of 9 modules at $50 per module or $400 for the whole series).
-
- For other course/training resources with certificates or CME/CEs:
- Visit the Telehealth Certification Institute
- Check out this free online course developed by Array on Telebehavioral Health Best Practices
- Visit the Telehealth Course Finder.
- For other course/training resources with certificates or CME/CEs:
-
- If you are a psychiatrist, here are some training opportunities specific to Telepsychiatry:
- Visit Telehealth Village for the Telemental Health - Introductory Module Telepsychiatry ($79 to take the module and includes CME/CE)
- Check out this free webinar on Telepsychiatry in the Era of COVID-19 developed in conjunction with the American Psychiatric Association and the Substance Abuse and Mental Health Services Administration (SAMHSA).
- If you are a psychiatrist, here are some training opportunities specific to Telepsychiatry:
- Now that I have the high level basics, what next?
- Visit the Clinical Guidelines section of our Telebehavioral Center of Excellence Website to start with, and then go on to explore the other sections! You'll find that we have curated many resources. Here are a few of the types of things you will find:
- The American Telemedicine Association in partnership with the American Psychiatric Association has put together Best Practices in Videoconferencing-Based Telemental Health (April 2018)
- The American Telemedicine Association has developed Practice Guidelines for Telemental Health with Children and Adolescents.
- The American Psychological Association has developed the following resources:
- The American Psychiatric Association has developed the following toolkits:
- The Inter Organizational Practice Committee (IOPC) has put together this Tele-Neuropsychology Toolkit that includes practice recommendations and guidelines, models, trainings and webinars and more.
- HHS has put together this Best Practice Guide: Telehealth for Behavioral Health Care
- If you do any kind of psychological assessments or testing, here are a few resources for you
- Visit the Clinical Guidelines section of our Telebehavioral Center of Excellence Website to start with, and then go on to explore the other sections! You'll find that we have curated many resources. Here are a few of the types of things you will find:
- What if I have patients/clients with specific clinical issues/needs?
-
- The Mental Health Technology Transfer Center Network funded by SAMHSA has a Clinical Innovations in Telehealth Learning Series, Sessions were recorded and posted online. Session topics include things like Telehealth and Suicide Care, Telehealth and CBTp for Psychosis, Providing Culturally Relevant Telehealth Services, and Treating PTSD.
-
- How should I manage a suicidal patient/client?
- Here is a learning session on Telehealth and Suicide Care:
-
- The Center for Practice Innovation has developed Telehealth Tips: Managing Suicidal Clients During the COVID-19 Pandemic. The document includes a Patient Safety Plan Template for you to use.
-
- This International Journal of Psychiatry in Medicine publication on Suicide Risk Management During Clinical Telepractice provides information about safety protocols and suicide risk assessment procedures used with U.S. military service members and veterans with depression.
- How should I manage victims of intimate partner/domestic violence or abuse?
- CASA is encouraging telehealth professionals to develop a code word to use when working with survivors to indicate if a perpetrator is in the room or within earshot. You would need to have done this in advance or during a time when you know for certain that the perpetrator is not around. For example, if you have met with a client and pre-arranged a code word (e.g., Walmart), and you notice a behavior change (or consider doing this at the start of every session), you could say following:
You: Have you gone to Walmart today?
Client: Yes (perpetrator is present), No (all clear)
You: Did you find what you needed?
Client: Yes (everything is fine and I am safe), No (please call 911 I am unsafe)
If they say yes then continue with your check in but do not go much deeper (e.g, avoid discussion of safety plans etc) so that you don’t tip the perpetrator off that you know they are there. In addition, if a Client brings up a statement about Walmart such as “I need to go to Walmart today”, it is an indicator that the perpetrator has walked in or is close by so you can begin to wrap things up.
-
- The National Network to End Domestic Violence has developed a number of resources:
- Using Technology to Communicate with Survivors During a Public Health Crisis, which also includes links to their Digital Services Toolkit on best practices for using tools such as text, chat and video
- The National Network to End Domestic Violence has developed a number of resources:
-
-
- Here is a video on COVID-19 & Survivor Confidentiality:
-
- How do I care for clients/patients who are in inpatient, residential or other non-ambulatory care settings?
- The American Psychiatric Association and the National Association for Behavioral Healthcare jointly hosted a recorded discussion with experts on How to Address COVID-19 Across Inpatient, Residential and Other Non-ambulatory Care Settings. The recording is available for free and CMEs are available (registration required).
- How do I care for clients/patients with serious mental illness?
- Here is a learning session on Telehealth and Cognitive Behavioral Therapy for Psychosis (CBTp):
-
- The American Psychiatric Association and the National Association for Behavioral Healthcare jointly hosted a recorded discussion with experts on Serious Mental Illness and COVID-19: Tailoring ACT Teams, Group Homes and Supportive Housing. The recording is available for free (registration required).
-
- Array is offering this online 1 CME credit training course on Treating Serious Mental Illness via Telepsychiatry free of charge during the pandemic.
-
- The Substance Abuse and Mental Health Services Administration (SAMHSA) as part of their Evidence-Based Resource Guide Series has developed Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders
- Are there any special considerations for working with rural populations, particularly the elderly?
- Array is offering this online 1 CME credit training course on Telepsychiatry for Rural Elderly free of charge during the pandemic.
(Hot Tip: Due to the overwhelming interest and need for telehealth during this pandemic, using the online form will generally get you a quicker response than calling and leaving a voicemail message. It is much more difficult to return calls after hours and on weekends, but we CAN respond to your emails. The more specific you are with your question or request (e.g., what type of provider you are, what type of setting you work in, what you specifically need), the better we will be at getting you timely and useful information.)
Getting Started with Remote Patient Monitoring
- Help me understand remote patient monitoring?
- Check out this brief under a minute introductory video taken from our Remote Patient Monitoring Toolkit on our website. This toolkit is dedicated to helping providers get started. Visit the toolkit and make sure you download the actual RPM Toolkit (it's an 8 page PDF document with lots of great information).
- What are some use cases for remote patient monitoring? There are many ways the remote patient monitoring is being used. Here are a few examples:
- The American Heart Association has issued Using Remote Patient Monitoring Technologies for Better Cardiovascular Disease Outcomes Guidance
- The Personal Connected Health Alliance has put together this article on Understanding Remote Patient Monitoring in COPD
- The Rural Health Information Hub has this spotlight on Telehealth Invigorating and Innovating Diabetes Care
- mHealth Intelligence published an article on Telehealth Gives Patients a Real-Time Link to Mental Health Support
- The California Health Care Foundation published this paper on Remote Patient Monitoring in the Safety Net: What Payers and Providers Need to Know
- What kinds of devices can be used for remote patient monitoring?
- The US Food & Drug Administration (FDA) has issued a new policy that allows manufacturers of certain FDA-cleared non-invasive vial sign-measuring devices to expand their use so that health care providers can use them to monitor patients remotely. The devices include those that measure body temperature, respiratory rate, heart rate and blood pressure.
Digital Health Literacy, Device Equity and Broadband Access Resources
- Telehealth Access for Seniors provides seniors and low-income communities with devices, instructions and free tech-support to connect them to their physicians via telehealth through the generosity of donations and volunteers. Visit their website to donate, request technical support (individuals) or to request assistance with accessing phones/tablets for your patients (clinics only).
- The National Digital Equity Center advocates for Digital Inclusion which includes Affordable Broadband, Affordable Equipment and Public Computer Access. The National Digital Equity Center is focused on creating digitally literate citizens across Maine and beyond, providing communities with the expertise to mobilize broadband technologies through digital inclusion and literacy efforts. While many of the resources are focused on Maine, there are also many educational resources applicable to all including online webinars/classes.
- COVID Tech Connect was founded with a mission to connect critically ill COVID-19 patients with their loved ones by donating smart devices to hospitals and care facilities across the country. They are currently offering 5-15 devices per facility, giving priority to those in greatest need.
- iCanConnect, also known as the National Deaf-Blind Equipment Distribution Program (NDBEDP), was established by the Federal Communications Commission (FCC). iCanConnect provides free equipment including smartphones, tablets, computers, screen readers, braille displays, and more to people who meet federal disability and income guidelines.
- National Assistive Technology Act Technical Assistance and Training (AT3) Center is your one-stop connection to information about the Assistive Technology Act, State Assistive Technology Programs, and general assistive technology and has this Program Directory of State Assistive Technology Programs.
- Telehealth Equity Coalition is building a wide coalition of supporters to advocate for greater access to telehealth, with a specific focus on broadband and hardware access, digital and health literacy, trust and accountability, social determinants of health, educating communities about telehealth and evidence and value based care.
- Digitunity (Digital Opportunity Network) is working to eliminate the technology gap in partnership with a network of stakeholders. While not focused on health care, some of their initiatives include refurbishing computers and creating pathways to device ownership.
- Cellular/Wireless Service: All four of the major United States carriers have signed on to the FCC’s Keep Americans Connected Pledge. Under this agreement, carriers have agreed to take the follow action for at least the next 60 days: 1) Not terminate service to any residential or small business customers because of their inability to pay their bills due to the disruptions caused by the coronavirus pandemic; 2) Waive any late fees that any residential or small business customers incur because of their economic circumstances related to the coronavirus pandemic; and 3) Open its Wi-Fi hotspots to any American who needs them.
- AT&T is currently offering home internet wireline customers unlimited data. New customers who are eligible for public assistance programs can subscribe to Access from AT&T for two months of free service. All public WiFi hotspots are open to anyone who needs them. AT&T will not terminate service of any wireless, phone or broadband residential or small business customer due to an inability to pay your bill. All late payment fees will be waived.
- Verizon will not charge late fees or terminate service to customers who are experiencing hardships because of COVID-19 and cannot pay their bill in full.
- Sprint is providing unlimited data for 60 days to customers with metered data plans effective 3/18/20.
- T-Mobile is providing customers on smartphone plans unlimited data for 60 days effective 3/13/20. Customers should dial 611 on their T-Mobile phone if they have concerns about bill payments due to COVID-19.
- Internet Service: In response to the coronavirus pandemic and its impact on society, multiple Internet Service Providers (ISPs) have made updates to their low-cost internet service programs to ensure individuals and families stay connected to the internet.
- To find low-cost Internet Service and Computers in Your Area, use this tool from everyoneon!
- The Affordable Connectivity Program: Helps low-income households pay for internet service and connected devices. If your household is eligible, you can receive: 1) up to $30/month discount on your internet service; 2) up toe a $75/month discount if your household is on qualifying Tribal lands and 3) a one-time discount of up to $100 for a laptop, tablet or desktop computer (with a co-payment of more than $10 but less than $50). A household is eligible if:
- Your household income is 200% or less than the Federal Poverty Guidelines.
- You participate in certain government assistance programs, such as SNAP, Medicaid, WIC, SSI, FPHA, Veterans Pension and Survivors Benefits, Free and Reduced-Price School Lunch Program or School Breakfast Program or received a Federal Pell Grant in the current award year.
- You live on qualifying Tribal lands of if someone in your household participates in Bureau of Indian Affairs General Assistance; Head Start; Tribal TANF or Food Distribution Programs on Indian Reservations.
- You already receive a Lifeline Benefit.
- If your child or dependent participates in the Free and Reduced-Price School Lunch Program or is enrolled in a USDA Community Eligibility Provision school.
-
- It was recently brought to our attention that the Halo Cellular Gateway might be a budget friendly (relatively speaking) way to bring broadband to areas with limited or no broadband access.
- Other Creative Solutions: While helping those who can't afford broadband to access it is useful if there is cellular or cable of fiber solution, there still remain areas in the U.S. that simply do not have this infrastructure. Some creative ways to help people access the internet that have been used include:
- Making available wi-fi access from schools, libraries, and other business parking lots so that individuals can access the wi-fi from their cars or even retro-fitting library study rooms or un-used spaces in schools to provide private spaces.
- Developing public wi-fi access points in the community such as in an abandoned store fronts or other un-used community facilities.
- Putting in kiosks with devices in areas of the community that do have broadband access.
- Check out this example from the Delaware Libraries: https://technical.ly/delaware/2021/05/11/delaware-libraries-telehealth-kiosks/ They are using this for their kiosk: https://www.talkboxbooth.com/. For those who want more information about the library initiative, here are two webinars:
Telehealth and HIPAA
- Give me the quick and dirty basics about HIPAA and Telehealth
- For a quick introduction to HIPAA Compliance and Telehealth, watch this brief video:
-
- You might also want to check out this HIPAA & Telehealth Infographic
- Is it true that I don't have to worry about HIPAA during the pandemic? Since most of you are frantically trying to get started yesterday, if you don't currently have any technology that you could use for a telehealth visit, please know that as part of its response to the pandemic, a change was made regarding HIPAA. The HHS Office for Civil Rights (OCR) is exercising enforcement discretion and waiving penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype. See FAQs on Telehealth and HIPAA during the COVID-19 Nationwide Public Health Emergency.
The intent of the OCR response to the pandemic is for providers to act responsibly and to make every effort to comply ("in good faith") with HIPAA in terms of technology selection and communications channels. This is particularly important when working with patients who might have sensitive health information. If you are using everyday communications technologies without encryption on a public wi-fi network, this is extra risky and you need to seriously weigh the risks against the benefits. If the situation is urgent/emergent, and you don't have other methods, by all means. However, if the situation is less urgent and you can arrange for a platform with encryption and/or move to a more private setting, you would be strongly advised to do so. With that said, please check your State policies, as not every state has waived enforcement of their HIPAA requirements.
-
- To check your State policies, Click Here, select the state of interest and then scroll down to the lower half of the page to see the original guidance documents and any new guidance related to COVID-19. Alternatively, just go up to the top menu bar and select your state under "Our Region".
-
- If you are considering using everyday communications technologies during this pandemic, the Health Information Technology Evaluation and Quality Center (HITEQ) has put together a very nice Issue Brief on Using non-traditional technology for telehealth during COVID-19 Pandemic that would be worth your time to review.
- What's all this news about Zoom-Bombing and what is the risk to privacy and security? While the "free" version of Zoom is not recommended for telehealth visits (there is a paid health care version that has more of the elements required by HIPAA), we know many of you are using it as a stopgap measure or for administrative meetings. In order to make Zoom user friendly, Zoom had set its "default" settings to be as open as possible. The majority of the issues you've heard/read about in the media were related to users not bothering to make adjustments to these default settings. This article on How to Prevent Zoom-Bombing provides some very practical information on how to mitigate the majority of the risks. Since this time, Zoom has updated their platform several times, changing many of the problematic default settings to more secure default settings.
- Are there any privacy/security issues related to using bluetooth headphones or other bluetooth devices for telehealth? Bluetooth can be a privacy/security risk. Bluetooth is an open standard for short-range radio frequency communication. If your mobile device has Bluetooth capability, turn off or set the Bluetooth connection capabilities to “nondiscoverable.” When in discoverable mode, Bluetooth-enabled mobile devices are “visible” to other nearby devices, which may alert a hacker to target them. When Bluetooth is turned off or in nondiscoverable mode, the Bluetooth-enabled mobile devices are invisible to other devices not authorized to access or monitor the data in your device. It is definitely not advisable to use Bluetooth in a public place or with a public network. Additionally, as with passwords, you should never share your Bluetooth pairing codes with anyone. For more information, take a look at this NIST Guide to Bluetooth Security.
- What do I need to know about HIPAA and audio only/telephone visits? The FCC issued a Declaratory Ruling and Order to clarify HIPAA rules and how they apply to telephone calls with patients. A very good summary of the rule may be found here. The enforcement discretion and waiver of penalties granted by OCR in response to the pandemic also applies to landline and wireless communications.
- I am trying to prepare for telehealth post-pandemic. What do I need to know about HIPAA and Telehealth? Here are several resources that can be used to help you prepare to do your own risk assessment:
- HIPAA Compliance Roadmap (Created by Behavioral Health Innovation)
- Telehealth Compliance Checklist (Created by Foley & Lardner, LLP)
- Telehealth Audit Checklist (Created by eCatalyst)
Working with Vendors (Technology and Service Providers)
- How do I got about selecting a vendor for telehealth technology or services? If you have a budget for technology and infrastructure and the luxury of taking a little time, we would recommend your using our Vendor Selection Toolkit.to better help you determine your technology and/or clinical requirements before selecting a vendor(s).
- There are so many technologies out there. How do I figure out what will meet my clinical requirements?
- The National Telehealth Technology Assessment Resource Center (TTAC) has put together a number of Toolkits to assist you with learning the fundamentals of the various technologies and how to assess those technologies. They have also created an Innovation Watch section that takes a closer look at new technologies as they come to market.
- Available Toolkits (includes a Clinician's Guide to Video Platforms)
- Innovation Watch
- The National Telehealth Technology Assessment Resource Center (TTAC) has put together a number of Toolkits to assist you with learning the fundamentals of the various technologies and how to assess those technologies. They have also created an Innovation Watch section that takes a closer look at new technologies as they come to market.
- How do I know what types of vendors are out there? If you are exploring what types of vendors are out there:
-
- If you are looking for telehealth service providers, the Southwest Telehealth Resource Center has put together this Service Provider Directory for Telemedicine and Telehealth.
- If you are looking for telehealth companies, Becker's Hospital Review has put together this list of 260+ Telehealth Companies to Know
Free/Low Cost Telehealth Technology Solutions and Services
Critical Care: The National Emergency Tele-Critical Care Network is a joint program of the U.S. Department of Health & Human Services (HHS) and the U.S. Department of Defense (DoD). It is available at no cost to hospitals caring for COVID-19 patients and struggling with access to enough critical care physicians, nurses, respiratory therapists, and other specialized clinical experts. Teams of critical care clinicians are available to deliver virtual care through telemedicine platforms, such as an app on a mobile device. Hear from participating clinicians, and click here to request assistance. Communications
- Significantly reduced pricing on Updox Secure Text for 6 months.
- Free Presence Scheduling and Telemedicine Solution
- Instant Language Assistant (Medical) software/app temporarily available to providers free during the pandemic.
- Free sign language Virtual Remote Interpretation by linguabee for COVID-19 test sites
- Free access to Safety Net Connect eConsult Telehealth Portal for primary care physicians
- Free access to ConferMED Coronavirus eConsults for Safety Net Practices
- Free access to The MAVEN Project for eConsults for community health clinics who serve the underserved.
- Free access to RubiconMD for 120+ specialties for qualifying safety net clinicians. Clinic leadership should contact covid19support@rubiconmd.com
- AireHealth Portable Nebulizer Kit on sale at significantly reduced rate with additional $25 off first nebulizer kit and free shipping with code WELCOME25
- Eko Telehealth is giving health systems 30 days of complimentary access to their stethoscope live streaming software and cardiac screening AI platform.
- Free access to Vivovitals remote patient monitoring platform for providers in the United States
- Significantly reduced pricing on Connected Healthcare Solutions (CHS) Health Guidance Platform for remote monitoring (reduced one time startup fee with no minimum quantities or contractual requirements - and use as many or as few devices as you need with no additional cost)
- LSI Rentals and Leasing Options offers both short and longer term rental and leasing options for patient monitoring equipment
- Free 90 day trial of KangarooHealth intelligent remote patient monitoring platform by contacting Bridget Holm
- Free use of Orbita COVID-19 Screening Chatbot & Knowledge Base through June 2020
- Hospitals can add for free Bright.md's coronavirus screening tool, based on its asynchronous virtual care delivery platform, SmartExam, to their websites. The online tool guides patients through a dynamically adaptive online medical interview, reviewing their symptoms and health history, as well as possible exposure to COVID-19.
- findhelp has a search platform that is free and open to help locate free and reduced-cost program resources to meet social need.
- Unite Us has a digital technology platform that connects organizations to each other to track referrals and outcomes. Community network partners (e.g., housing services, food assistance, behavioral health etc) can join for free.
- Free trial of Vyopta Platform for automating compliance reporting and system utilization and capacity monitoring for hospitals and health systems scaling up to 1K end users or more.
- Free 60 day trial access to Bluestream virtual care platform
- Free temporary access to Compunetix Video Call Center for Healthcare platform with no fees or obligations
- Free white-labeled RingMD telemedicine platform for doctors, healthcare groups and other organizations negatively affected by the outbreak.
- Free Cloudbreak Health unified telemedicine and video medical interpretation solution app with free service for hospitals
- Free Allm JOIN platform in the ED and JOIN Triage to EMS/ambulance providers to facilitate quick assessment, routing to appropriate hospital, pre-notification to destination hospital, bi-directional communication including video calls. Works in conjunction with radio and other existing systems.
- Free basic and significantly reduced pricing on full featured Adaptive Telehealth telemental health platform license
- Free standard plan (supported by promotions and advertising) through Vivadox
- Free basic doxy.me telemedicine platform
- Free basic doximity temedicine platform
- Free TeleHome video call platform designed for to help caregivers connected isolated COVID-19 patients with loved ones on any device, anywhere.
- $3 pay per use plan (other plans available) and free imaging with Nautilus Medical Technologies teleray video & audio communication and dicom image exchange solution.
- Free trial access to CompuGroup Medical US CGM ELVI web-based video platform
- Free Pulsara ONE + COVID-1g video-enabled platform to all EMS and healthcare organizations
- Significantly reduced pricing on Updox Video Chat for 6 months.
 BEST PRACTICES FOR CONDUCTING A TELEHEALTH VISIT
BEST PRACTICES FOR CONDUCTING A TELEHEALTH VISIT
Developing Policies, Procedures and Protocols
- Policies define your practices' position on what you plan to do and why you plan to do it. It is generally pretty brief. For example, is your policy to temporarily address urgent care needs with telehealth and to delay non-urgent care visits in response to COVID-19? Or is your policy to develop a comprehensive strategy for addressing all patients' needs, as appropriate, using telehealth technologies that will be sustainable beyond COVID-19?
- Procedures describe how a policy will be put into action across all aspects of your operations. Procedures define roles and responsibilities regarding things like who will do what, what forms will be used, what will need to be documented, and any limits to professional discretion. You will want to develop procedures regarding the scheduling of telehealth visits, paperwork and documentation requirements, when and how to make referrals for lab tests, etc.. For example, if a patient calls to cancel an appointment because they want to mitigate exposure to the virus, who will they be speaking with when they call? Will that person offer the patient the option of a telehealth visit? If your policy is to only schedule urgent care issues via telehealth and not routine wellness checks, then what will staff need to look for (e.g., appointment.visit type) or ask the patient to determine if the scheduled visit was urgent vs. non-urgent?
- Protocols define particular sets of operating procedures and are sometimes accompanied by workflow diagrams. Protocols define the order of operations and the specific tasks and expectations, serving as a formal agreement and commitment between two or more parties.
- The American Telemedicine Association has developed Operating Procedures for Pediatric Telehealth.
- The Federation of State Medical Boards has established a Model Policy for the Appropriate Use of Telemedicine Technologies in the Practice of Medicine. This document was designed for State licensing boards, but is actually an excellent way to think about policies and procedures within an organization or practice.
- This draft Sample Telehealth Policies and Procedures was developed by an actual organization (they have given us permission to strip the identifiers and to share).
Thinking About Workflow
- This less than 10 minute video snippet will help you think about a few considerations that may impact your workflow as you get started. These are considerations related to both the patient and provider experience:
- If time allows, the National Consortium of Telehealth Resource Centers (NCTRC) hosted a webinar on Mapping and Designing Telehealth Clinic Workflows, with a more in-depth focus on how to develop workflow diagrams for your team.
- The following are some key questions to discuss with your team as you develop your workflow:
- How will my patient/client be informed about the availability of telehealth services? Who will tell them? What will they be told? How will they be told? When will they be told?
- How will telehealth visits be scheduled and who will do the scheduling? When will each clinician be available for telehealth visits (e.g., only during specific blocks of times or on specific days or scheduled like any other office visit or always available)?
- How will the patient/client be prepared and who will prepare them? What information will the provider need before the visit? How does this differ for new vs. established patients/clients? What paperwork is needed and who will collect/how will this be collected? Will reminders be sent? If so, when and by whom?
- How will your patient/client be informed about how to use the technology? Who will help the patient/client or the provider with technical or connection issues?
- Where will the provider be during visits? Is their location private and secure? Is there adequate bandwidth? How will the provider access and interface with the EMR? Will the provider need dual monitors?
- How will the provider know when the patient/client is ready to be seen? Will there be a virtual waiting room? What will the patient see/hear as they wait? How will communication take place if the provider or patient/client is running late?
- What will happen at the end of the visit? Will there be some kind of follow up? Who will follow up? How will the visit be documented and by whom? How will the visit be billed and by whom?
- How will staff be trained and by whom? How will you onboard new staff?
- The following are sample workflows for a variety of settings that can serve as a starting point and then customized to fit your specific situation(s) and needs:
-
- Outpatient
- We have put together a few sample workflow templates for your use:
- Outpatient
-
-
- The American Academy of Pediatrics has provided Swimlane Workflow Diagrams (see Appendix A) for Provider-Patient (after hours), Provider-Patient (during office hours) and for Provider to Other Medical Facility/Office.
-
-
-
- CaravanHealth has developed:
- This set of flow charts/diagrams looks at Re-Engineering Patient Inflow and looks at Triaging Incoming Visit Types to the Best Virtual Visit Types
- Telehealth E/M Workflow Diagram
- CaravanHealth has developed:
-
-
-
- This draft Sample Telehealth Policies and Procedures includes a workflow diagram.
-
-
-
- The Center for Care Innovations has put together Telehealth and Telephone Visits in the Time of COVID-19: FQHC Workflows and Guides. While these were collected from FQHC settings, the sample workflows would be broadly applicable in other clinic settings as well.
-
-
-
- The Upper Midwest TRC has developed this Patient-Provider Telehealth Workflow
-
-
-
- The California TRC has developed:
-
-
-
- Virginia Health Catalyst has developed this Teledentistry Workflow
-
-
- Inpatient/Facility
- West Health has developed this Telehealth Workflow for Post-Acute and Long Term Care Facilities
- Inpatient/Facility
-
-
- VCU Health has developed this Inpatient Telemedicine Process with Example iPhone Patient Room Setup
-
Thinking About Consent
- Is informed consent for telehealth required? Medicare does not require that informed consent be obtained from a patient prior to a telehealth visit, but Medicare reimburses for a set of Virtual Communications Services that they do not consider "telehealth". For these services, there is an informed consent requirement (learn more about Telehealth vs. Virtual Communication Services in our section in this toolkit on Telehealth Reimbursement and COVID-19). Additionally, many states either require informed consent within their Medicaid program or in their statute or rules regulating health professionals. Some states define very specific required elements within the consent process. To find out if and what your state requires in terms of consent, click here and then follow the instructions below:
- Select your state of interest from the State dropdown box at the top of the webpage.
- Policies regarding consent may be located in multiple sections.
- First, click on the COVID-19 box and select "Easing Consent Requirements" to see if there have been any temporary changes due to the public health emergency.
- Next, click on the Medicaid box and select "Consent Requirements" to see if there are any specific requirements by the funder.
- Finally, click on Professional Requirements and click on "Consent Requirements" to see if there are any specific requirements by the professional licensing board.
MATRC maintains guidance documents related to state Medicaid programs and SOME health professions regulations and guidance documents for states in the MATRC coverage area. To see if what you might be looking for is available on our website, Click Here to select the state of interest and then scroll down to the lower half of the page to see the various State policy guidance documents. Alternatively, go up to the top menu bar and select the state of interest under “Our Region”.
- What goes into telehealth consent? In telehealth, informed consent is used to explain what telehealth is, lay out the expected benefits and possible risks associated with it, and explain security measures. We think it's good practice to get consent, whether it is required or not.
The Federation of State Medical Boards has established a Model Policy for the Appropriate Use of Telemedicine Technologies in the Practice of Medicine. In this document, they recommend the inclusion of the following when getting consent for telehealth:
-
- Identification of the patient, the physician and the physician’s credentials;
- Types of transmissions permitted using telemedicine technologies (e.g. prescription refills, appointment scheduling, patient education, etc.);
- The patient agrees that the physician determines whether or not the condition being diagnosed and/or treated is appropriate for a telemedicine encounter;
- Details on security measures taken with the use of telemedicine technologies, such as encrypting data, password protected screen savers and data files, or utilizing other reliable authentication techniques, as well as potential risks to privacy notwithstanding such measures;
- Hold harmless clause for information lost due to technical failures; and
- Requirement for express patient consent to forward patient-identifiable information to a third party.
If you are not a physician, your particular profession (or professional organization) may have guidance about consent and recommended elements of consent as well.
- How often do I need to obtain consent and does it need to be written consent? Requirements may vary by State. Unless your State and/or State Medicaid program explicitly requires the consent form to be signed (most places do not), it may be done verbally. Unless your State and/or State Medicaid program specifically requires you to obtain consent before every visit (most places do not or are not explicit about frequency), it may be done once (or preferably once a year). Medicare in the PHE waiver explicitly says a single consent per year is needed, and that it may be done verbally. It is recommended that you have a written process (by whom and when) and protocol (with script) developed that is considered standard operating procedure. Make sure you date the protocol and include a revision date each time it is revised. Once that is in place, in most cases, you just need to document in the medical record that your consent process/protocol (include the version date) was used and that the patient provided consent.
- Do you have some sample consent form templates? Following are several sample consent forms for a variety of practice types. You will need to adapt these forms to your clinical use case and your state's policy requirements. You may not need every element or you may need to add elements.
-
- Here is a sample General Consent Form in English and a sample General Consent Form in Spanish (credit goes to California TRC).
-
- Here is a sample Telemedicine Program Consent Form (credit goes to Southwest TRC)
-
- The Agency for Healthcare Research and Quality (AHRQ) has created a sample Easy to Understand Telehealth Consent Form. The form includes language for healthcare providers that have curtailed in-person visits due to COVID-19. AHRQ has also created how-to guidance for clinicians on how to obtain informed consent for telehealth.
-
- Here is a sample Telemental Health Informed Consent Form in English and a sample Telemental Health Informed Consent Form in Spanish developed by the National Association of Social Workers.
-
- Here is a sample Telepsychology Informed Consent Form developed by the Joint Task Force for the Development of Telepsychology Guidelines for Psychologists
Documenting a Telehealth Visit
- Patient's location (with enough detail to satisfy a Medicare audit, i.e., eligible facility in an eligible geographic location).
- There have been many exceptions made during this pandemic as a result of the different waivers, so this is not as important during the state of emergency, but in general you should do this so you might as well make it a practice!
- If the patient's home is the location of service, and the address is already somewhere in the medical record, then you just need to include in your note that the visit took place at the patient's home. You do not need to capture the address again.
- It is always good practice to verify the patient's location at the start of every virtual visit. Do not assume they are at home! Remember that if the patient experiences an emergency/crisis when they are in the middle of a visit with you, if you don't have easy access to the address of their physical location (a PO Box will not work), it will be impossible to contact first responders and have them deployed to the patient's location.
- We have encountered situations where the patient is actually traveling (e.g, in a car) during a telehealth visit. Should this be the case, note that the patient was in a vehicle, but do ask what State the patient is in. Note this in the patient record to ensure documentation of compliance with any licensure requirements.
- Provider's location (under normal circumstances, this would be the usual place of practice – for most, it would be the office location, but if home is a routine or the only office location, then the provider’s home location should be registered as a site of service and used). With that said, please note that during the period of the COVID-19 emergency declaration, CMS is allowing physicians and other practitioners to render telehealth services from their home without reporting their home address on their Medicare enrollment form while continuing to bill from their currently enrolled location(s).
- That the encounter was conducted via telehealth (defined by both audio and visual communication). If the visit did not include both audio and visual communication, one should specify what other means were used (telephone, patient portal, etc.)
- Start and stop time/total time (documentation for billing requires total time spent by the physician or other qualified health care professional on the date of encounter for all activities related to that patient and/or the medical decision-making). If the total time spent with the patient/client is via telehealth, you can simply document the start and stop time of the telehealth visit. Otherwise, you should document total time spent on the date of encounter, inclusive of all other activities pertaining to the patient and/or the medical decision-making. Some payers may want the actual start/stop time of the telehealth visit in addition to the total time, so it doesn't hurt to document both.
- That the patient consented (unless otherwise documented). Please refer to your State's laws/licensing board regulations and guidance documents regarding specific requirements. See section on consent above for how to do this.
- Any other providers involved or individuals present, including telepresenters and family members.
- Optional: A reason for using telehealth (medical or otherwise), and any criteria used to evaluate whether the case was appropriate for telehealth. If the visit was audio-only (telephonic), it is recommended that a reason be provided (e.g.., no internet access, no access to video enabled device, could not get technology to work, etc.)
Telehealth Etiquette
- What is telehealth etiquette? Telehealth etiquette, sometimes referred to as "webside manner" is an important, but often overlooked contributor to the overall patient experience with telehealth. Interacting through telehealth technology requires some attention to detail that may be different than the in-person encounter. Following is an outstanding quick video for providers to capture some of the most important best practice elements of videconferencing etiquette.
Video developed by the State of Hawaii Department of Health Genomics Section and Western States Regional Genetics Network (UH7MC30774-01-00) in collaboration with the Pacific Basin Telehealth Resource Center.
If time allows, explore this FREE Telehealth Etiquette Video Series developed by the South Central TRC. It provides an excellent introduction to how a telehealth encounter should (and should not) be conducted! If you have never seen or participated in a telehealth encounter, we would strongly recommend running through these very real life situations. In addition, download the following which has several very practical checklists:
Additionally, here are two checklists on telehealth etiquette that you might find useful. We recommend printing one of these out and having it with you as you get started with telehealth visits. Take notes and add/adapt it as you discover new lessons learned!
-
- Telehealth Etiquette Checklist.
- Telehealth Visit Etiquette Checklist (American Medical Association)
- What about telephone etiquette? The American Academy of Family Physicians has developed two good resources for those conducting telephone visits:
Clinical Assessment and the Physical Exam
- Are there any practice guidelines for providing clinical care using telehealth?
- The American Telemedicine Association (ATA) has developed Practice Guidelines for Live, On Demand Primary and Urgent Care.
-
- Depending on the type of provider you are and the type of service you offer, there are other specific clinical guidelines and best practices for telehealth that have been developed. The ATA has some of these other practice guidelines in their Practice Guidelines Archive.
-
- In response to the pandemic, Harvard Medical School is waiving tuition for their online course on The Telephone & Telemedicine in Clinical Medicine: An Instrument of Opportunity & Risk (includes 3 AMA PRA Category 1 Credits).
- How do I perform a physical exam by telehealth? Following are some great resources to help you with this!
- This article "Why the Telemedicine Physical is Better than You Think" gives some great perspective as well as some very practical ideas about what can be done even without peripheral devices.
-
- ODU's Center for Telehealth Innovation, Education and Research (C-TIER) has developed Telehealth training videos. The focus of this series is on physical exams via Telehealth. Several of these videos show how practitioners instruct the patient in a self-exam with the use of a tablet and/or computer, along with a series of questions. Other videos in this series show how practitioners can use various Telehealth devices to conduct physical exams and consult with specialists.
- Telehealth Physical Exam: ENT
- ODU's Center for Telehealth Innovation, Education and Research (C-TIER) has developed Telehealth training videos. The focus of this series is on physical exams via Telehealth. Several of these videos show how practitioners instruct the patient in a self-exam with the use of a tablet and/or computer, along with a series of questions. Other videos in this series show how practitioners can use various Telehealth devices to conduct physical exams and consult with specialists.
-
-
- Telehealth Physical Exam: Skin
-
-
-
- Telehealth Physical Exam: Abdominal
-
-
-
- Telehealth Physical Exam: Cardiopulmonary
-
-
-
- Telehealth Physical Exam: Neurological
-
-
-
- Telehealth Physical Exam: Musculoskeletal
-
-
-
- Introduction to Conducting Physical Exams via Telehealth with Devices
-
-
-
- Conducting a Pediatric Well-visit using a Mobile Telehealth Device
-
-
-
- Using Remote Patient Monitoring (RPM) Equipment to Assess Congestive Heart Failure
-
-
-
- Mobile Telehealth Device used to Assess Back Pain between Nurse Practitioner and Specialist
-
-
-
- Telehealth Robot Assists Nursing Facility Staff Communicate Assessment with Primary Care Provider
-
-
-
- Pre-op Airway Assessment via a Telehealth Cart and Oral Camera
-
-
- If you want to kill two birds with one stone, this is an excellent online training developed by Thomas Jefferson University Sidney Kimmel Medical College on Telemedicine: Conducting an Effective Physical Exam Online Course ($100 for this 1 hour online course that includes CME/CE)
-
- CaravanHealth has developed detailed guidance on the Telehealth Physical Exam as well as detailed guidance on Adapting the Annual Wellness Visit to Telehealth
-
- The American Academy of Ophthalmology has developed this guidance on the Home Eye Test for Children and Adults. This website guidance page also includes downloadable home eye testing charts.
- What if I am using the telephone?
- The CDC has developed Phone Advice Line Tools: Guidelines for Children or Adults with Possible COVID-19. This document includes initial phone scripts, accompanying decision algorithm and tailored care advice messages.
-
- In response to the pandemic, Harvard Medical School is waiving tuition for their online course on The Telephone & Telemedicine in Clinical Medicine: An Instrument of Opportunity & Risk (includes 3 AMA PRA Category 1 Credits).
Meeting the Needs of Patients/Clients Who Need Interpreters or Have Disabilities
- Section 504 of the Rehabilitation Act of 1973 – applies to federal health care services and facilities; and health care providers who are also recipients of federal financial assistance, usually provided by direct funding (such as federal Medicaid funds) or by grants (such as a federal research grant).
- Title II of the Americans with Disabilities Act – applies to all public (state and local) health care providers.
- Title III of the Americans with Disabilities Act – applies to all private health care providers.
- Things to consider when weighing your options:
- Video interpretation, when possible, will be a better option than audio only because the majority of communication is done nonverbally!
- A trained healthcare interpreter will almost always be better than using staff, family or friends. Some patients will insist on using family members or friends. Don't be afraid to offer an alternative if you have one.
- Here are a few resources you may want to review:
- If you have access to a trained healthcare interpreter:
- There are many videoconference platforms that allow for multi-point videoconferencing. There is no reason not to continue to use your interpreter remotely by video.
- As an example, Zoom for Healthcare has a built-in feature that allows you to add an interpreter as well as a closed captioning and live transcription. While Zoom has a pilot integration with otter.ai for artificial intelligence driven transcription, it is not recommended for important healthcare communications due to the often technical vocabulary being used. If you do use this feature, please monitor and correct errors continuously and carefully. To find a Communication Access Realtime Translation (CART) provider (real-time captioning or live-event captioning), please visit the National Court Reporter's Association Sourcebook and search for CART Captioning services.
- There are many videoconference platforms that allow for multi-point videoconferencing. There is no reason not to continue to use your interpreter remotely by video.
- If you don't have access to a trained healthcare interpreter:
- The National Board of Certification for Medical Interpreters has a searchable registry of interpreter training programs. These programs may be able to direct you to certified medical interpreters in your state. These individuals may or may not have had training in video/remote interpretation.
- There are some telehealth platforms that have integration of healthcare interpreter services (both language and AS:L) as part of their license agreement with end-users.
- Examples of such platforms include ViTelNet and Cloudbreak
- There are remote interpretation companies that provide interpretation by video.
- Examples of such companies include Stratus Video/InDemand Interpreting and LanguageLine Solutions. You will likely find many others with a simple search. Make sure you ask for someone who is trained in healthcare interpretation. .
- Do not use Google Translate for important healthcare communications. Google Translate has only 57.7% accuracy when used for medical phrase translation! If you have no other options and can't reschedule the visit at a time when an interpreter is available, a somewhat better alternative would be the Instant Language Assistant app being made temporarily available to providers for free during the pandemic.
- If you are an interpreter or know one that has never done interpretation by video before:
- Please take a look at our Telehealth Etiquette video resources found in our section on Best Practices for Conducting a Telehealth Visit in this COVID-19 Resource toolkit..
- The National Council on Interpreting in Health Care has a number of good resources, including these two webinars:
- Temporary Transition to Remote Interpreting During Health Emergencies: Guidance and Tips for Language Access Stakeholders (recorded webinar is free for NCIHC members and $30 for non-members, but slides and FAQs may be accessed for free by all)
- The Critical Role of Healthcare Interpreters During the COVID-19 Pandemic: Legal and Practical Implications (free live webinar on April 25, recording will be free for NCIHC members and at cost for non-members)
- How do I help my non-English speaking patients understand and prepare for a telehealth visit?
- In response to the increased use and expanded coverage of telehealth during the COVID-19 pandemic, From Coverage to Care (C2C) has released new resources to support patients and providers in making the most of virtual care. They have developed a guide called Telehealth: What to Know for Your Family. It is available in eight languages: English (PDF), Arabic / ال عرب ية (PDF), Chinese / 中文 (PDF), Haitian Creole / Kreyòl Ayisyen (PDF), Korean / 한국어 (PDF), Russian / Русский (PDF), Spanish / Español (PDF), Vietnamese / TIẾNG VIỆT (PDF)
- How do I help my non-English speaking patients navigate technology?
- What are the specific considerations for patients/clients with disabilities? Here is a nice graphic developed by the Northwest Regional TRC that answers this question:
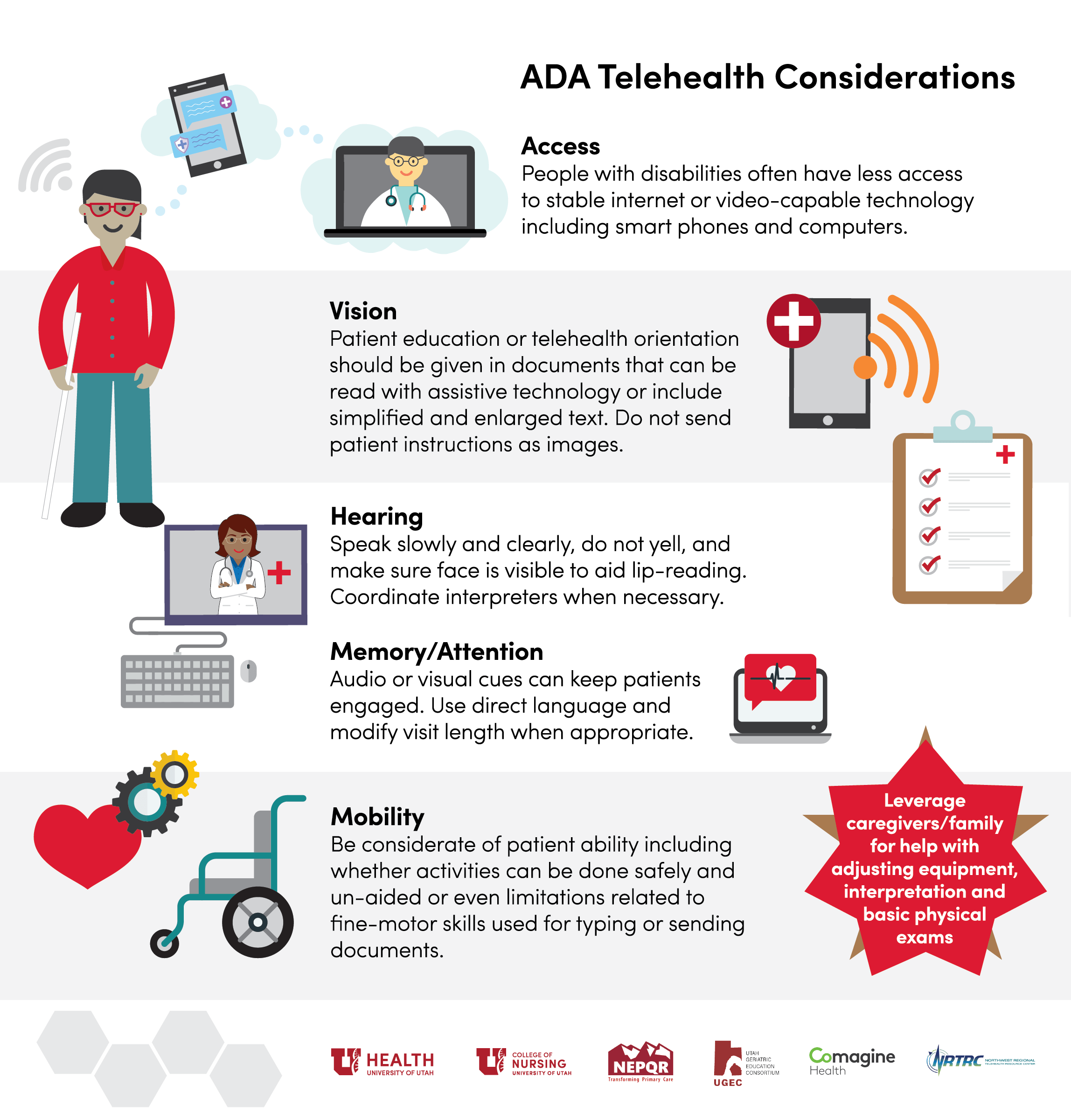
- What kind of auxiliary aids and services are required by the ADA to ensure effective communication with individuals with hearing or vision impairments?
- The ADA National Network has compiled a really nice list of appropriate auxiliary aids and services.
- What if I have a deaf or hard of hearing patient? The options mentioned above for language services would also apply to interpretation for those who are deaf or hard of hearing, including most, if not all of the examples of platform and interpretation service providers/vendors. Additionally, below are some specific best practice for this population with special needs:
- The National Association of the Deaf has developed the following resources:
-
- Hearing Loss Association of America has developed the following resources:
-
- The North Carolina Department of Health and Human Services has created several excellent telehealth guidance documents for Healthcare Providers:
-
- If you are an ASL interpreter, the Southwest Telehealth Resource Center hosted this webinar on ASL Interpreters (on video or in person) in Medical Settings and the Law that might be of interest. Although some of the materials are specific to Arizona, much of it is relevant to all ASL interpreters.
-
- Free sign language is being offered by Virtual Remote Interpretation by linguabee for COVID-19 test sites during the pandemic.
-
- iCanConnect, also known as the National Deaf-Blind Equipment Distribution Program (NDBEDP), was established by the Federal Communications Commission (FCC). iCanConnect provides free equipment including smartphones, tablets, computers, screen readers, braille displays, and more to people who meet federal disability and income guidelines.
-
- National Assistive Technology Act Technical Assistance and Training (AT3) Center is your one-stop connection to information about the Assistive Technology Act, State Assistive Technology Programs, and general assistive technology and has this Program Directory of State Assistive Technology Programs.
Educating the Patient About Telehealth
- What can I give or share with my patients/clients to help them understand telehealth?
- Here are a few infographics and patient resources that can help patients better understand what a telehealth visit
-
-
- How Patients Can Engage Telehealth:
-
-
-
- Telebehavioral Health (this was created by the Upper Midwest TRC and provides a brief overview of Telebehavioral Health)
-
- Do you have a script for me to use to explain telehealth and virtual care to my patients/clients?
- The South Central TRC has developed this tip sheet: How to Engage Your Patients in Telemedicine
-
- CaravanHealth has developed these two templates that you can use to help you communicate with your patients about telehealth and other types of virtual visits:
- How do I help my patients/clients understand about the need for an internet connection and learn about the technology needed for a telehealth visit?
- Family Voices received 2020 CARES Act funds to support telehealth for families of children with Special Health Care Needs. Many of these resources are broadly applicable to all families.
- "Are You Connected Webinar" to help families with children with special health care needs to understand the basics about getting and improving their cellular or WiFi connection. They have also developed the following infographics for addressing common barriers to connectivity:
- Family Voices received 2020 CARES Act funds to support telehealth for families of children with Special Health Care Needs. Many of these resources are broadly applicable to all families.
-
-
- "Do You Have a Device Webinar" to help families with children with special health care needs to understand that computers, laptops, tablets and smartphones can all be used for a telehealth visit and to learn if their device is "teleready". They have also developed the following infographic:
-
-
-
- "Can You 'See' Your Provider Webinar" to help families learn the keys for a successful family centered telehealth appointment. They have also developed the following infographics:
-
-
- Telehealth Access for Seniors has developed a large number of easy to understand downloadable Tech Guides that may be useful. Their website includes guides for Gmail Setup, Wifi, MyChart App, MyChart Website, Apple-ID Setup, Android Device, Amazon Fire and Play Store. There are also several guides in Spanish, Korean, Chinese and Arabic.
- How can I help my patient/client be prepared for a telehealth visit?
-
- Here is an outstanding video for patients developed by the State of Hawaii Department of Health Genomics Section and Western States Regional Genetics Network (UH7MC30774-01-00) in collaboration with the Pacific Basin Telehealth Resource Center to help patients understand telehealth, what to expect and how to prepare.
-
- We (MATRC) wrote this article on How to Help a Family Member or Friend with Their First Telehealth Visit for Senior Navigator.
-
- In response to the increased use and expanded coverage of telehealth during the COVID-19 pandemic, From Coverage to Care (C2C) has released new resources to support patients and providers in making the most of virtual care. They have developed a guide called Telehealth: What to Know for Your Family. It is available in eight languages:
-
- The California Telehealth Resource Center has developed this Infographic: How Do I Use Telehealth? Frequently Asked Questions and Insights for Patients
-
- Doctors Technology Office has developed this Virtual Care Frequently Asked Questions for patients to prepared them for a visit along with troubleshooting tips.
-
- The American Psychiatric Association and SAMHSA has developed this infographic on How to Prepare for a Video Appointment with Your Mental Health Clinician.
-
- The Center of Excellence for Protected Health Information through funding by SAMHSA has developed this Infographic on Tips to Keep Your Telehealth Visit Private. This has some very practical advice for patients/clients related to protecting communications, creating the right environment and protecting their devices.
-
- The South Central TRC has created this infographic on Make the Most of Your Telemedicine Visit: For Patients. This easy to follow three-pager providers an excellent overview for patients on what is telehealth, why use telehealth, what to expect from a visit and how to prepare for a visit.
-
- The Upper Midwest TRC has created this infographic about Your Telemedicine Appointment. This easy to understand one-pager providers an excellent overview for patients on how to prepare for an appointment.
-
- All in for Health and The Children's Partnership have developed this Fact Sheet on Telehealth + Children: Frequently Asked Questions
-
- Family Voices has developed "Your Family's First Telemedicine Appointment Webinar" to help families of children with Special Health Care Needs prepare for a successful family centered telehealth visit. They have also developed the following infographics:
 RESOURCES FOR SPECIALTY PROVIDERS AND SETTINGS
RESOURCES FOR SPECIALTY PROVIDERS AND SETTINGS
Specialty and Setting Specific Guidance Documents
- Here you will find links to medical and advanced practice nursing specialty specific guidance developed by different professional associations/organizations:
- The American Academy of Dermatology has developed this Teledermatology Toolkit
-
- The American Academy of Neurology has put together the following resources:
- Telemedicine and COVID-19 Implementation Guide
- Telemedicine and COVID-19 FAQ
- NeuroBytes: The Neurologic Exam Via Telemedicine training course that is free to AAN members
- NeuroLearn: Introduction to Teleneurology training course that is free to AAN members and for a fee for nonmembers that includes 1.0 CMEs..
- The American Academy of Neurology has put together the following resources:
-
- The American Academy of Pediatrics has provided a number of Sample Documents, including a Telehealth Visit Protocol, Patient Recruitment Sample Letter, Swimlane Workflows and Start-up Checklist for Connecting a Specialist to a Private Practice. In addition, they have developed this webinar on Telehealth and COVID-19.
-
- The American Association of Nurse Practitioners has developed this training on Telehealth: What Nurse Practitioners Need to Know that is free to AANP members and for a fee for nonmembers that includes CE Credits.
-
- The American College of Cardiology put together this podcast: Practice Made Perfect: Telehealth Ensuring Quality Cardiovascular Care During Uncertain Times.
-
- The American College of Physicians has developed An ACP Physician's Guide that has a section on telehealth, has developed a curriculum called Telemedicine: A Practical Guide for Incorporation into your Practice and has put together this webinar on Revving Up Your Telemedicine Practice in the Time of COVID.
-
- The American Diabetes Association has developed this webinar on Telehealth and COVID-19
-
- The American Medical Association has developed a "Quick Guide to Telemedicine in Practice" that has a section on Practice Implementation.
-
- The American Society of Cataract and Refractive Surgery has developed this webinar on Implementing Tele-Ophthalmology During COVID-19 Pandemic
-
- The American Urological Association has put together this white paper on Telemedicine in Urology as well as a number of other valuable resources in their Telemedicine Info Center for COVID-19.
-
- The Association of Community Cancer Centers has developed a resource page on Coronavirus Response for Cancer Care.
-
- The Federal Interagency Committee on EMS has developed this Telemedicine Framework for EMS and 911 Organizations.
-
- The National Rural Health Resource Center partnered with the Northwest Regional Telehealth Resource Center to develop this Critical Access Hospital Telehealth Guide.
-
- The Providers Clinical Support System (PCSS) has developed FAQs for Treating Opioid Use Disorder via Telehealth Tips for Primary Care Providers
-
- The Society of Critical Care Medicine has developed this "Tip Sheet: Application of Telemedicine and Telecritical Care to Emergency Management of COVID-19
Teledentistry
- What is exactly teledentistry and how will this help me during COVID-19 and Beyond?
- Check out these these resources for a nice overview!
- American TeleDentistry Association Facts About Teledentistry
- CareQuest Institute for Oral Health:
- Teledentisty: What to Know & How It Works
- Teledentistry: Providing Access to Care During the Covid-19 Crisis
- Using Teledentistry to Maintain Services and Contact with Patients During COVID-19
- Approaches for Prioritizing Care in Response to COVID-19
- Expanding Oral Health: Teledentistry
- Teledentistry Use Beyond the Pandemic
- Check out these these resources for a nice overview!
-
- Now take a look at this webinar by Dr. Paul Glassman on Teledentistry and Minimally Invasive Procedures in the Time of COVID-19:
- How do I get started?
- The National Network for Oral Health Access (NNOHA) has developed this Teledentistry Learning Collaborative Teledentistry User Guide.
-
- Virginia Health Catalyst has developed these very practical tools along with the following video showing a practice teledentistry visit for dentists getting started::
- American Teledentistry Association Guidelines for Teledental Practice
- Crisis Teledentistry Implementation Guide (a few of the pages are specific to Virginia policies, but but the rest of the document has great information about teledentistry practice recommendations and resources)
- Teledentistry Workflow Chart
- Practice Teledentistry Visit Video:
- Virginia Health Catalyst has developed these very practical tools along with the following video showing a practice teledentistry visit for dentists getting started::
-
- Teledent has put together this guidance document on Patient Assessment via Synchronous Teledentistry
-
- The American Dental Association (ADA) has put together this Guide to Understanding and Documenting Teledentistry Events.
-
- CareQuest Institute for Oral Health has put together this great teledentistry etiquette video on Answering that Dental Emergency Call Remotely:
- The American Teledentistry Association has put together this Industry Standards for Remote Orthodontic Treatment
- CareQuest Institute for Oral Health has developed some very nice resources for providers to give to their patients:
Telegenetics
Here are some additional resources that you might find useful as well:
- The National Coordinating Center for the Regional Genetics Networks has a Telemedicine/Telehealth Resource Page that has a great resource repository.
- The National Genetics Education and Family Support Center has developed a patient facing infographic called TELEWHAT?: An Introduction to Telegenetics that might be useful for you or provide your patients..
Telehealth and Autism Care
- The Council of Autism Service Providers has developed a number of resources:
- Practice Parameters for Telehealth-Implementation of Applied Behavior Analysis
- Organizational Guidelines & Standards
- Webinar on Autism Telehealth in Crises and Beyond
- Webinar Video (free but registration required)
- Webinar Slides
- Behaviorbabe has a great website on ABA and Telehealth. Following is video about ABA, Telehealth and COVID19 from their website (many more videos and other resources on the website as well):
- There is a Telehealth in ABA Facebook Group with some great ideas. It is a private group so you will need to request to join.
- The Behavioral Health Center of Excellence has developed the following webinars to assist providers:
- K-Now Solutions has put together this webinar on Telehealth in ABA: The Building Blocks
- Psych Central has this reflection post on Tele-ABA Activities for Kids: 7 Telehealth Activities ABA Providers Can Use with Children with ASD
- Insight + Regroup is offering this online 1 CME credit training course on Telepsychiatry and Children with Autism Spectrum Disorder free of charge during the pandemic.
- Professionals in Italy developed this paper on a Model of Support for Families of Children with Autism Living in the COVID-19
- This is an excellent blog post on 10 Strategies for Engaging Parents (not Children?) during Tele-Intervention
- MSU Autism Lab hosted this webinar on Parent Coaching through Telehealth:
- Behavior Development Solutions has developed a course on Coaching Caregivers Through the Internet; Challenges and Solutions for Successful Telehealth Services. There is a small fee for the course, but 1.5 BACB Learning CE credits are being offered.
- Family Voices received 2020 CARES Act funds to develop a host of resources to support telehealth for families of children with Special Health Care Needs. Visit their website to see training resources, toolkits and more. Many of these resources are detailed in our section on Educating the Patient About Telehealth.
You may also want to visit our section of resources on Telerehabilitation, Telepractice and Early Intervention Services!
Telehealth for Post-Acute and Long-Term Care Settings and Services
- West Health, in partnership with the AARP and the National Consortium of Telehealth Resource Centers has put together this webinar on The Use of Telehealth in Long Term Care Settings During this National Emergency (click here for Powerpoint slides)
- West Health has also developed a number of resources for PALTC settings:
- Getting Started with Telehealth: PALTC
- Getting Started with Telehealth: Provider (with PALTC)
- A Practical Guide to Telehealth: Implementing Telehealth in Post-Acute and Long-Term Care Settings (PALTC)
- Rapid Deployment: Getting Started with Telehealth Pre-visit Form: PALTC
- Rapid Deployment: Getting Started with Teleheallth Post-visit From: PALTC
- Telehealth Workflow for Post-Acute and Long Term Care Facilities
- The Society for Post-Acute and Long-Term Care Medicine has published Standards for the Use of Telemedicine for Evaluation and Management of Resident Change of Condition in the Nursing Home
- The American Psychological Association has put together How to Provide Telehealth in Nursing Homes, with tips for offering essential psychological services to older residents during the pandemic.
- Altarum recently released a report entitled Rapid PACE Responses in a Covid-19 Era: How PACE Providers Have Innovated and Adapted to Keep Enrollees Safe in Their Communities.
- LeadingAge has developed a number of guides for the selection and implementing of technologies:
- Telehealth and Remote Patient Monitoring for Long-Term and Post-Acute Care: A Primer and Provider Selection Guide
- Social Connectedness and Engagement Technology for Long-Term and Post-Acute Care: A Primer and Provider Selection Guide
- Safety Technology for Long-Term and Post-Acute Care: A Primer and Provider Selection Guide
- Medication Management Technologies for Long-Term and Post-Acute Care
- Electronic Health Records (EHRs) for Long-Term and Post-Acute Care: A Primer on Planning and Vendor Selection
- Functional Assessment and Activity Monitoring Technology: A Primer and Provider Selection Guide
- Shared Care Planning and Coordination Technology for Long Term and Post-Acute Care: A Primer and Provider Selection Guide
- Resident/Client Technology Support and Training Guide
Telehospice and Telepalliative Care
- The Center to Advance Palliative Care has put together a comprehensive Telehealth and Palliative Care Toolkit with both downloadable guidance documents and web-based resources in the following areas:
- Setting Up a Program
- Preparing Patients and Families
- Conducting Telehealth Visits: Etiquette
- Conducting Telehealth Visits: Remote Physical Examination
- Telehealth Documentation and Billing
- The Journal of Palliative Medicine as published an article on Top Ten Tips Palliative Care Clinicians Should Know About Telepalliative Care
- The National Hospice and Palliative Care Organization (NHPCO) has put together a number of excellent resources:
- The Shiley Haynes Institute for Palliative Care has put together a 4 hour self-paced online course that includes 4 CE/CME Credits on Telemedicine Skills for Clinicians. Total cost of the course is $79.In addition, they have made available the following recorded Six Session Telemedicine Now (and How!) Connecting at a Distance Open Forum Series:
-
- Session 1: Effectiveness and Connection via Telemedicine: Getting Past the (Real and Imagined) Hurdles
-
- Session 2: Expert Q&A on Symptom Management and Patient Education at a Distance
-
- Session 3: Virtually Anything in COVID-19: The Many Uses of Technology for Caring
-
- Session 4: Best Practices for Hosting Sensitive Conversations by Video
-
- Session 5: Boundaries and Intimacy: How Deeply Can We Connect at a Distance?
-
- Session 6: Emergency Medicine, Nursing Home Residents, and Tele-Palliative Care: Past, Present, and Future
- :The National Care Planning Council has put together About Telehospice Care as part of their Guide to Long Term Care Planning.
- Husch Blackwell has developed this Hospice Telehealth Flowchart: How to Provide Medically Necessary Hospice Physician and Nurse Practitioner Visits via Telehealth to Medicare Hospice Patients During the COVID-19 Pandemic
- The Association of Professional Chaplains has developed is A Quick Guide to Providing Telechaplaincy Services
Telerehabilitation, Telepractice and Early Intervention Services
- Physical Therapy:
- The American Physical Therapy Association has put together a number of telehealth resources. Here is just a sampling:
-
- The Federation of State Boards of Physical Therapy Guidelines: Telehealth in Physical Therapy
-
- The Family, Infant and Preschool Program has put together this infographic for Physical Therapists on Tele-Move: I'm a PT, Don't Take My Hands Away From Me
-
- The Inspired Treehouse has some great and mostly free child development resources for parents and professionals, including a set of digital therapy games. Many of the free resources can be used virtually.
-
- There are a few vendors that have developed some technology based solutions for Physical Therapy applications that may be of interest to some.
Please note that MATRC is not in a position to either endorse or recommend any of the above vendors. We strongly encourage you to do your due diligence when making a vendor selection. There may be other vendors with a PT specific focus, these are simply ones that have been brought to our attention thus far.
- Occupational Therapy:
- The American Occupational Therapy Association has put together a number of telehealth resources. Here is just a sampling:
-
- The American Congress of Rehabilitation Medicine as put together this webinar on Telehealth Resources for Occupational Therapy
-
- OTPotential has developed this informative Telehealth Occupational Therapy Guide that you might also find useful.
-
- The Family, Infant and Preschool Program has put together this infographic for Occupational Therapists on Tele-Sense: Making Sense of Sensory Preferences
- Telepractice/Telespeech:
- The American Speech-Language-Hearing Association (ASHA) has put together a number of resources on telepractice. Here is just a sampling:
-
- We have a recorded webinar on "Innovation and Impact with Speech Language Pathology Telepractice
-
- SpeechPathology.com offers a two-part course on Pediatric Telepractice with CEUs for $99/year: Telepractice: What You Need to Know for Practical Applications in Pediatrics and Telepractice: Day in the Life of a Teletherapist, the Inside Scoop
-
- Pearson Assessments provides a brief How To on Telepractice and a video demo of Q-global Quick Look Demo for Speech Language Pathologists for conducting the CELF-5 and GFTA Assessments.
-
- The Family, Infant and Preschool Program has put together this infographic on Tele-Speech: SLPs, Can We Talk? Our Virtual Role
- Early Intervention Services (you may also want to visit our earlier section of resources on Telehealth and Autism Care):
- The Family, Infant and Preschool Program (FIPP) has put together an amazing set of resources on Early Childhood Intervention Telepractice, including a set of Tele-Practie Infographics and this video on Providing Early Intervention Services Through Distance Technology:
-
- The Infant and Toddler Connection of Virginia put together this Teleflections Video Series which provides reflections from Virginia early intervention service providers on tele-intervention:
- Teleflections Video 1 – My First Online Visit
- Teleflections Video 2 – Tele-What?!
- Teleflections Video 3 - Bandwidths, Platforms, and Pings?? Help!
- Teleflections Video 4 - I'm a PT and Rely on my Hands
- Teleflections Video 5 – Woke Up Worried
- Teleflections Video 6 - Mom was Over the Moon
- Teleflections Video 7 - Update from Julie
- Teleflections Video 8: Getting Creative in Rural Areas
- The Infant and Toddler Connection of Virginia put together this Teleflections Video Series which provides reflections from Virginia early intervention service providers on tele-intervention:
They also hosted this webinar on Telepractice in Early Intervention:
-
- This document has some very practical information on Planning for the Use of Video Conferencing for Early Intervention Home Visits during the COVID-19 Pandemic
-
- ASHA offers several resources on early intervention services. These include:
- Using Telepractice to Provide Early Intervention Services to Families
- Online Conference Session (free to members) on The State of Telepractice for Delivering Early Intervention Services
- ASHA offers several resources on early intervention services. These include:
-
- Sweet Pea Pediatric Wellness has made available this video on Getting Started with Telehealth for Early Intervention Providers - Tips & Tricks
-
- The Early Childhood Technical Assistance Center has put together a presentation on Use of Tele-Intervention in Early Intervention (IDEA Part C): Strategies for Providing Services Under the COVID-19 Public Health Emergency
-
- The National Center for Hearing Assessment and Management has put together A Practical Guide to the Use of Tele-Intervention in Providing Early Intervention Services to Infants and Toddlers Who Are Deaf or Hard of Hearing
-
- Family Voices received 2020 CARES Act funds to develop a host of resources to support telehealth for families of children with Special Health Care Needs. Visit their website to see training resources, toolkits and more. Many of these resources are detailed in our section on Educating the Patient About Telehealth as well as our section on Best Practices for Conducting a Telehealth Visit, subsection on "What Should I Do If My Patient/Client Needs an Interpreter"
- Telehealth Technology specific to telerehabilitation for Speech, OT, PT, ABA and more are available and can make help facilitate care. While MATRC cannot endorse or recommend any particular vendors, below is just a sampling of a few things available in the market.
*Please exercise due diligence whenever making decisions about technologies and vendors. Consult with our Vendor Selection Toolkit and take advantage of our Virtual Office Hours related to Technology and Vendors if you need some assistance navigating the technology and vendor space!
Tele-Substance Use Disorder Treatment and Recovery Services
- View our conference session on Behavioral Health and Substance Use Disorder: Telehealth Implementation and Practice Considerations: This session will help you understand how a behavioral health organization quickly implemented telehealth practices during COVID-19 and address billing and coding, approaches to inpatient and outpatient care, explore differences between telephonic and video telehealth and identify innovative ways to adjust workflows to meet patient needs.
- The Addiction Technology Transfer Center (ATTC) Network, funded by SAMHSA has developed the following resources:
-
- Telehealth Learning Series for SUD Tx and Recovery Support Providers (live one-hour sessions each week with access to experienced providers, training tools, checklists and more). There is an archive of recorded past session materials.
- SBIRTcolorado.org has developed this outstanding guidance document on Screening, Brief Intervention, Referral to Treatment (SBIRT & Telehealth)
- We have, as part of our Telebehavioral Health Center of Excellence website, a page of general MAT and Tele-MAT Resources
- The Providers Clinical Support System (PCSS) has developed FAQs for Treating Opioid Use Disorder via Telehealth Tips for Primary Care Providers
- The DEA has provided this Policy Guidance documents:
- The Center of Excellence for Protected Health Information has developed this slideset from a webinar on Understanding the New SAMHSA/OCR Guidance for Telehealth SUD and MH Services
- The National Council for Behavioral Health made available this recorded COVID-19 Office Hour session focused on Opportunities for Peer Support Workers, Supervisors and Programs
- The Center for Connected Health Policy has put together this report on Barriers & Challenges to FQHC Use of Telehealth for Substance Use Disorder: A Examination of Policies Affecting FQHCs Pre- and During COVID-19 Emergency.
- The Substance Abuse and Mental Health Services Administration (SAMHSA) as part of their Evidence-Based Resource Guide Series has developed Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders
 TELEHEALTH POLICY AND COVID-19
TELEHEALTH POLICY AND COVID-19
Impact of COVID-19 on Federal and State Policies
- For a summary the array of policy changes as a result of the pandemic, visit: COVID-19 Telehealth Coverage Policies
- For more information, including a searchable database by topic and by state, visit Telehealth in the Time of COVID-19.
- If you are a licensed psychologist, the American Psychological association has also tracked State Actions Relevant to Licensed Psychologists During COVID-19.
- The US Health and Human Services must officially renew the public health emergency (PHE), a status that allows many of the waivers and expansions for telehealth that have occurred since the COVID-19 pandemic began in March 2020 to remain active. Each renewal extends the PHE an additional 90 days. The latest renewal, which occurred on April 13, 2022 extends the PHE through July 11, 2022.
Licensure, Interstate Practice and Credentialing/Privileging
- Licensure Exemptions Under the 4th Amendment to the Declaration under the PREP Act- Medical Countermeasures Against COVID-19. On December 3, 2020, the US Department of Health and Human Services (HHS) issued a fourth amendment to the Declaration Under the Public Readiness and Emergency Preparedness Act (PREP Act) for Medical Countermeasures Against COVID-19. In the amendment was the inclusion of a telehealth provider under the “covered person” designation. The amendment further noted that if a telehealth provider was delivering a “covered countermeasure” via telehealth to a patient in a state the telehealth provider was not licensed it, state laws, including state licensure requirements, that prohibited such actions would be pre-empted. A telehealth provider who is not licensed in the state the patient is located in, will be able to provide a select set of services without having to be licensed. However, there are certain qualifications and parameters that must be met. Read this Fact Sheet to better understand which situations would allow for licensure exemption.
- Patients/Clients From Multiple States See Me In My Office. May I Continue to See Them Using Telehealth During This Pandemic? In general, a clinician must be licensed in the state where the patient/client is physically located at the time of service. Former President Trump declared an emergency on March 13, 2020. As a result, the Centers for Medicare & Medicaid Services (CMS) has authorized the 1135 Waiver that took effect retroactively to March 1, 2020. This waiver is limited in scope to conditions of participation and payment for Federal health care programs such as Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP). Authorization of this waiver alone DOES NOT waive the requirement for physicians and other healthcare providers to maintain licensure in states where they are practicing a licensed profession, including via telehealth. What the waiver does is that it gives States the option of being able to do so. State law continues to govern whether a provider is authorized to provide professional services in that state without holding an active license from that state’s medical board. Many state medical and other health professions licensing boards have created mechanisms that either waive or expedite state licensure requirements in response to the pandemic.
- We Work with College or University Students and They Are Now Dispersed Throughout the Country. May I Continue to See Them or Assist Them? As mentioned earlier, in general, a clinician must be licensed in the state where the patient/client is physically located at the time of service. However, in conversations with multiple state licensing boards, most provide leniency around this when it comes to pre-existing relationships and continuity of care. Additionally, many state medical and other health professions licensing boards have created mechanisms that either waive or expedite state licensure requirements in response to the pandemic. If the state where your student is has not already made provisions for interstate practice during the pandemic, I would recommend contacting the licensing board for your health profession and just verifying that they will be OK with going across state lines to maintain continuity of care for a college student.
- On April 15, 2020, student representatives from over 130 universities across the country signed onto a Letter Addressed to the State Medical Licensing Boards for Mental Health Providers encouraging them to mandate an update on interstate licensing requirements so that mental health care providers can meet the needs of their students who happen to be residing in different states as a result of COVID-19. This is a developing issue that we will be monitoring.
- We work with a variety of non-physician health care practitioners. What do I need to consider when thinking about interstate telehealth practice? As mentioned earlier, in general, a clinician must be licensed in the state where the patient/client is physically located at the time of service. In additional to understanding the telehealth specific laws and rules in each state, there are a few other policy considerations that need to be researched and understood. A few of these include:
-
- Scope of practice laws: Each state has different policies related to Scope of Practice for different types of providers. If a practitioner is licensed in multiple states and is using telehealth to provide services across state lines, that practitioner needs to keep in mind what he/she may or may not do based on the laws of the state where the patient/client is located at the time of service. The NCSL Scope of Practice Policy website provides good information about Behavioral Health Providers, Nurse Practitioners, Oral Health Providers, Pharmacists and Physician Assistants by state. Please note that providers for some professions and in some states are required to have collaborative practice agreements with a physician. In this case, the collaborating physician must also be licensed in the State where the patient is physically located at the time of service.
- Malpractice coverage: The provider/practitioner (and collaborating physician if one is required) needs to check with their malpractice carrier to make sure they are covered for both telemedicine services (most do, but some require an additional rider) and that the coverage extends beyond state lines. Additionally, if it does extend beyond state lines, they also need to make sure that the malpractice coverage cap (or no cap) aligns with the different state’s malpractice policies. Different states have caps in widely varying amounts and others don’t have caps at all. The coverage needs to be adequate to meet all the different state requirements.
-
- Which state medical and other health professions licensing boards have created mechanisms that either waive or expedite state licensure requirements in response to the pandemic? Here are several professional organizations and associations that have been tracking changes to telehealth licensure policy during the pandemic:
-
- The Multi-Discipline Licensure Resource Project has been developed to serve as an information hub for Occupational Therapists, Physical Therapists, Psychologists and Social Workers
-
- Telemental Health Training Institute States' Rules and Regulations has a database by topic, including States' Responses to COVID-19. Specific for counselors, social workers, marriage and family therapists and psychologists.
- I hear that some states participate in interstate compacts for practitioners. Can you tell me more about those? As interstate practice through telehealth has expanded, many professions and states have developed efforts to facilitate interstate practice. The following are the compacts that have been developed (or are in process of being developed).
- APRN Compact: The APRN Compact allows an advanced practice registered nurse to hold one multistate license with a privilege to practice in other compact states. This compact has been adopted, but has not yet been implemented. It will be implemented once 7 states have enacted legislation for joining the compact.
- Audiology & Speech-Language Pathology Interstate Compact (ASLP-IC): The ASLP-IC facilitates the interstate practice of audiology and speech-language pathology while maintaining public protection.
- EMS Compact: The EMS Compact facilitates the day to day movement of EMS personnel across state boundaries in the performance of their EMS duties as assigned by an appropriate authority. The EMS Compact authorizes state EMS offices to afford immediate legal recognition to EMS personnel licensed in any other member state.
- Interstate Medical Licensure Compact (IMLC): The Interstate Medical Licensure Compact offers a voluntary, expedited pathway to licensure for qualified physicians who wish to practice in multiple states. Please note that this is not the same as reciprocity between participating states. Some states who do not participate in the Compact have a process called "Licensure by Endorsement" that also creates a more efficient/expedited process for a physician who is licensed and in good standing in one state to get licensed in another state.
- Nurse Licensure Compact (NLC) The Nurse Licensure Compact allows a nurse to have a multistate license with the ability to practice in their home state and all participating compact states. This is considered reciprocity between participating states.
- Psychology Interjurisdictional Compact (PSYPACT): PSYPACT is designed to facilitate the practice of telepsychology and the temporary in-person, face-to-face practice of psychology across state boundaries.
- Physical Therapy Compact (PT Compact): The PT Compact is an agreement between participating states that allows PTs and PTAs more mobility in where they practice.
For more information about which states participate in which compacts, you may check each of above compact websites or search by state at the CCHP Licensure Compacts Page.
The Council of State Governments has also developed a National Center for Interstate Compacts Database that serves as an information clearinghouse related to all interstate compacts in use today. This includes health professions, but is not specific to health professions.
Finally, Provider Bridge is a platform developed to streamline the process for mobilizing health care professionals during the COVID-19 pandemic and for future public health emergencies. It will offer a dedicated customer service hub to help clinicians navigate current state licensure requirements, including those specific to telehealth during states of emergency and provide access to a database of information for verified, betted, volunteer clinicians willing to provide telehealth services during emergencies.
CREDENTIALING AND PRIVILEGING- What does the Joint Commission Require in terms of Privileging when Providing Services Via Telehealth During a Disaster? The applicable requirements that address disaster privileging are found in the Emergency Management (EM) chapter of the Hospital and Critical Access Hospital Accreditation Manuals at EM.02.02.13. NOTE: The disaster privileging option ONLY applies when the organization has implemented their emergency management plan.
Licensed Independent Practitioners (LIP) CURRENTLY credentialed and privileged by the organization, who would now provide the same services via a telehealth link to patients, would not require any additional credentialing or privileging. The medical staff determines which services would be appropriate to be delivered via a telehealth link. There is no requirement that ‘telehealth’ be delineated as a separate privilege.
For volunteer Licensed Independent Practitioners that are NOT currently credentialed and privileged by the organization, disaster privileges may be granted to volunteer LIPs by following the requirements outlined in the Emergency Management chapter of the accreditation manual.
- Are there any CMS Waivers Related to Credentialing and Privileging of Medical Staff? CMS is waiving requirements under 42 CFR §482.22(a)(1)-(4) to allow for physicians whose privileges will expire to continue practicing at the hospital and for new physicians to be able to practice before full medical staff/governing body review and approval to address workforce concerns related to COVID-19. CMS is waiving §482.22(a) (1)-(4) regarding details of the credentialing and privileging process.
Prescribing of Controlled Substances
- Due to the declaration of a public health emergency, the Drug Enforcement Administration (DEA) has made changes to their policies regarding its rules related to prescribing. Review DEA Information on Telemedicine. With that said, please check your State policies, as many States also have laws and regulations governing telehealth and prescribing and these laws and regulations may not have been changes in response to COVID-19.
- Following is a decision tree summarizing the policy changes regarding How to Prescribe Controlled Substances to Patients During the COVID-19 Public Health Emergency
- Historic Background: The Ryan Haight Act of 2008 allowed for certain exemptions to the use of telehealth to provide controlled substances without the telehealth provider having seen the patient in-person first, however these exemptions are narrowly tailored. Two such exemptions are:
1. when a public health emergency (PHE) is declared, and 2. if a provider is registered on a telehealth registry that the Drug Enforcement Administration (DEA) will create.
Such a registry has never been established. In 2018, Congress passed the SUPPORT for Patients and Communities Act as part of an effort to combat the opioid epidemic. The Act directed the DEA to promulgate final regulations for the registry that would allow providers to prescribe controlled substances through telemedicine under certain circumstances. The DEA officially missed its deadline, set at one year from the passing of the Act on October 24, 2019.
-
- A December regulatory posting suggested the DEA plans to publish a proposal, however there was no definitive timeline outlined for the rule’s publication.
- The declaration of a Public Health Emergency (PHE) in March 2020 triggered an allowance in federal law that temporarily allows for the expanded use of telemedicine in prescribing controlled substances for the duration of the PHE. However, that allowance will expire at the end of the PHE.
- In response to the lack of action by the DEA and given the worsening opioid overdose crisis, the Alliance for Connected Care convened more than 80 organizations, who jointly signed a letter urging the DEA to move forward with the telemedicine special registration process required by federal law that will enable SAMHSA waivered clinicians, community mental health centers and addiction treatment facilities to prescribe medication assisted treatment (MAT) drugs to patients with OUD employing telemedicine technology. To read about the issue in more detail and view the letter, see the Alliance for Connected Care’s webpage on the issue.
- In May 2021, Senator Warner sent a letter to Attorney General Merrick Garland regarding the long-delayed regulations and expressed great concern for the delay.
Stay tuned for more updates!
Developing Policies, Procedures and Protocols
- Policies define your practices' position on what you plan to do and why you plan to do it. It is generally pretty brief. For example, is your policy to temporarily address urgent care needs with telehealth and to delay non-urgent care visits in response to COVID-19? Or is your policy to develop a comprehensive strategy for addressing all patients' needs, as appropriate, using telehealth technologies that will be sustainable beyond COVID-19?
- Procedures describe how a policy will be put into action across all aspects of your operations. Procedures define roles and responsibilities regarding things like who will do what, what forms will be used, what will need to be documented, and any limits to professional discretion. You will want to develop procedures regarding the scheduling of telehealth visits, paperwork and documentation requirements, when and how to make referrals for lab tests, etc.. For example, if a patient calls to cancel an appointment because they want to mitigate exposure to the virus, who will they be speaking with when they call? Will that person offer the patient the option of a telehealth visit? If your policy is to only schedule urgent care issues via telehealth and not routine wellness checks, then what will staff need to look for (e.g., appointment.visit type) or ask the patient to determine if the scheduled visit was urgent vs. non-urgent?
- Protocols define particular sets of operating procedures and are sometimes accompanied by workflow diagrams. Protocols define the order of operations and the specific tasks and expectations, serving as a formal agreement and commitment between two or more parties.
- The American Telemedicine Association has developed Operating Procedures for Pediatric Telehealth.
- The Federation of State Medical Boards has established a Model Policy for the Appropriate Use of Telemedicine Technologies in the Practice of Medicine. This document was designed for State licensing boards, but is actually an excellent way to think about policies and procedures within an organization or practice.
- This draft Sample Telehealth Policies and Procedures was developed by an actual organization (they have given us permission to strip the identifiers and to share).
Thinking About Workflow
- This less than 10 minute video snippet will help you think about a few considerations that may impact your workflow as you get started. These are considerations related to both the patient and provider experience:
- If time allows, the National Consortium of Telehealth Resource Centers (NCTRC) hosted a webinar on Mapping and Designing Telehealth Clinic Workflows, with a more in-depth focus on how to develop workflow diagrams for your team.
- The following are some key questions to discuss with your team as you develop your workflow:
- How will my patient/client be informed about the availability of telehealth services? Who will tell them? What will they be told? How will they be told? When will they be told?
- How will telehealth visits be scheduled and who will do the scheduling? When will each clinician be available for telehealth visits (e.g., only during specific blocks of times or on specific days or scheduled like any other office visit or always available)?
- How will the patient/client be prepared and who will prepare them? What information will the provider need before the visit? How does this differ for new vs. established patients/clients? What paperwork is needed and who will collect/how will this be collected? Will reminders be sent? If so, when and by whom?
- How will your patient/client be informed about how to use the technology? Who will help the patient/client or the provider with technical or connection issues?
- Where will the provider be during visits? Is their location private and secure? Is there adequate bandwidth? How will the provider access and interface with the EMR? Will the provider need dual monitors?
- How will the provider know when the patient/client is ready to be seen? Will there be a virtual waiting room? What will the patient see/hear as they wait? How will communication take place if the provider or patient/client is running late?
- What will happen at the end of the visit? Will there be some kind of follow up? Who will follow up? How will the visit be documented and by whom? How will the visit be billed and by whom?
- How will staff be trained and by whom? How will you onboard new staff?
- The following are sample workflows for a variety of settings that can serve as a starting point and then customized to fit your specific situation(s) and needs:
-
- Outpatient
- We have put together a few sample workflow templates for your use:
- Outpatient
-
-
- The American Academy of Pediatrics has provided Swimlane Workflow Diagrams (see Appendix A) for Provider-Patient (after hours), Provider-Patient (during office hours) and for Provider to Other Medical Facility/Office.
-
-
-
- CaravanHealth has developed:
- This set of flow charts/diagrams looks at Re-Engineering Patient Inflow and looks at Triaging Incoming Visit Types to the Best Virtual Visit Types
- Telehealth E/M Workflow Diagram
- CaravanHealth has developed:
-
-
-
- This draft Sample Telehealth Policies and Procedures includes a workflow diagram.
-
-
-
- The Center for Care Innovations has put together Telehealth and Telephone Visits in the Time of COVID-19: FQHC Workflows and Guides. While these were collected from FQHC settings, the sample workflows would be broadly applicable in other clinic settings as well.
-
-
-
- The Upper Midwest TRC has developed this Patient-Provider Telehealth Workflow
-
-
-
- The California TRC has developed:
-
-
-
- Virginia Health Catalyst has developed this Teledentistry Workflow
-
-
- Inpatient/Facility
- West Health has developed this Telehealth Workflow for Post-Acute and Long Term Care Facilities
- Inpatient/Facility
-
-
- VCU Health has developed this Inpatient Telemedicine Process with Example iPhone Patient Room Setup
-
Thinking About Consent
- Is informed consent for telehealth required? Medicare does not require that informed consent be obtained from a patient prior to a telehealth visit, but Medicare reimburses for a set of Virtual Communications Services that they do not consider "telehealth". For these services, there is an informed consent requirement (learn more about Telehealth vs. Virtual Communication Services in our section in this toolkit on Telehealth Reimbursement and COVID-19). Additionally, many states either require informed consent within their Medicaid program or in their statute or rules regulating health professionals. Some states define very specific required elements within the consent process. To find out if and what your state requires in terms of consent, click here and then follow the instructions below:
- Select your state of interest from the State dropdown box at the top of the webpage.
- Policies regarding consent may be located in multiple sections.
- First, click on the COVID-19 box and select "Easing Consent Requirements" to see if there have been any temporary changes due to the public health emergency.
- Next, click on the Medicaid box and select "Consent Requirements" to see if there are any specific requirements by the funder.
- Finally, click on Professional Requirements and click on "Consent Requirements" to see if there are any specific requirements by the professional licensing board.
MATRC maintains guidance documents related to state Medicaid programs and SOME health professions regulations and guidance documents for states in the MATRC coverage area. To see if what you might be looking for is available on our website, Click Here to select the state of interest and then scroll down to the lower half of the page to see the various State policy guidance documents. Alternatively, go up to the top menu bar and select the state of interest under “Our Region”.
- What goes into telehealth consent? In telehealth, informed consent is used to explain what telehealth is, lay out the expected benefits and possible risks associated with it, and explain security measures. We think it's good practice to get consent, whether it is required or not.
The Federation of State Medical Boards has established a Model Policy for the Appropriate Use of Telemedicine Technologies in the Practice of Medicine. In this document, they recommend the inclusion of the following when getting consent for telehealth:
-
- Identification of the patient, the physician and the physician’s credentials;
- Types of transmissions permitted using telemedicine technologies (e.g. prescription refills, appointment scheduling, patient education, etc.);
- The patient agrees that the physician determines whether or not the condition being diagnosed and/or treated is appropriate for a telemedicine encounter;
- Details on security measures taken with the use of telemedicine technologies, such as encrypting data, password protected screen savers and data files, or utilizing other reliable authentication techniques, as well as potential risks to privacy notwithstanding such measures;
- Hold harmless clause for information lost due to technical failures; and
- Requirement for express patient consent to forward patient-identifiable information to a third party.
If you are not a physician, your particular profession (or professional organization) may have guidance about consent and recommended elements of consent as well.
- How often do I need to obtain consent and does it need to be written consent? Requirements may vary by State. Unless your State and/or State Medicaid program explicitly requires the consent form to be signed (most places do not), it may be done verbally. Unless your State and/or State Medicaid program specifically requires you to obtain consent before every visit (most places do not or are not explicit about frequency), it may be done once (or preferably once a year). Medicare in the PHE waiver explicitly says a single consent per year is needed, and that it may be done verbally. It is recommended that you have a written process (by whom and when) and protocol (with script) developed that is considered standard operating procedure. Make sure you date the protocol and include a revision date each time it is revised. Once that is in place, in most cases, you just need to document in the medical record that your consent process/protocol (include the version date) was used and that the patient provided consent.
- Do you have some sample consent form templates? Following are several sample consent forms for a variety of practice types. You will need to adapt these forms to your clinical use case and your state's policy requirements. You may not need every element or you may need to add elements.
-
- Here is a sample General Consent Form in English and a sample General Consent Form in Spanish (credit goes to California TRC).
-
- Here is a sample Telemedicine Program Consent Form (credit goes to Southwest TRC)
-
- The Agency for Healthcare Research and Quality (AHRQ) has created a sample Easy to Understand Telehealth Consent Form. The form includes language for healthcare providers that have curtailed in-person visits due to COVID-19. AHRQ has also created how-to guidance for clinicians on how to obtain informed consent for telehealth.
-
- Here is a sample Telemental Health Informed Consent Form in English and a sample Telemental Health Informed Consent Form in Spanish developed by the National Association of Social Workers.
-
- Here is a sample Telepsychology Informed Consent Form developed by the Joint Task Force for the Development of Telepsychology Guidelines for Psychologists
Documenting a Telehealth Visit
- Patient's location (with enough detail to satisfy a Medicare audit, i.e., eligible facility in an eligible geographic location).
- There have been many exceptions made during this pandemic as a result of the different waivers, so this is not as important during the state of emergency, but in general you should do this so you might as well make it a practice!
- If the patient's home is the location of service, and the address is already somewhere in the medical record, then you just need to include in your note that the visit took place at the patient's home. You do not need to capture the address again.
- It is always good practice to verify the patient's location at the start of every virtual visit. Do not assume they are at home! Remember that if the patient experiences an emergency/crisis when they are in the middle of a visit with you, if you don't have easy access to the address of their physical location (a PO Box will not work), it will be impossible to contact first responders and have them deployed to the patient's location.
- We have encountered situations where the patient is actually traveling (e.g, in a car) during a telehealth visit. Should this be the case, note that the patient was in a vehicle, but do ask what State the patient is in. Note this in the patient record to ensure documentation of compliance with any licensure requirements.
- Provider's location (under normal circumstances, this would be the usual place of practice – for most, it would be the office location, but if home is a routine or the only office location, then the provider’s home location should be registered as a site of service and used). With that said, please note that during the period of the COVID-19 emergency declaration, CMS is allowing physicians and other practitioners to render telehealth services from their home without reporting their home address on their Medicare enrollment form while continuing to bill from their currently enrolled location(s).
- That the encounter was conducted via telehealth (defined by both audio and visual communication). If the visit did not include both audio and visual communication, one should specify what other means were used (telephone, patient portal, etc.)
- Start and stop time/total time (documentation for billing requires total time spent by the physician or other qualified health care professional on the date of encounter for all activities related to that patient and/or the medical decision-making). If the total time spent with the patient/client is via telehealth, you can simply document the start and stop time of the telehealth visit. Otherwise, you should document total time spent on the date of encounter, inclusive of all other activities pertaining to the patient and/or the medical decision-making. Some payers may want the actual start/stop time of the telehealth visit in addition to the total time, so it doesn't hurt to document both.
- That the patient consented (unless otherwise documented). Please refer to your State's laws/licensing board regulations and guidance documents regarding specific requirements. See section on consent above for how to do this.
- Any other providers involved or individuals present, including telepresenters and family members.
- Optional: A reason for using telehealth (medical or otherwise), and any criteria used to evaluate whether the case was appropriate for telehealth. If the visit was audio-only (telephonic), it is recommended that a reason be provided (e.g.., no internet access, no access to video enabled device, could not get technology to work, etc.)
Telehealth Etiquette
- What is telehealth etiquette? Telehealth etiquette, sometimes referred to as "webside manner" is an important, but often overlooked contributor to the overall patient experience with telehealth. Interacting through telehealth technology requires some attention to detail that may be different than the in-person encounter. Following is an outstanding quick video for providers to capture some of the most important best practice elements of videconferencing etiquette.
Video developed by the State of Hawaii Department of Health Genomics Section and Western States Regional Genetics Network (UH7MC30774-01-00) in collaboration with the Pacific Basin Telehealth Resource Center.
If time allows, explore this FREE Telehealth Etiquette Video Series developed by the South Central TRC. It provides an excellent introduction to how a telehealth encounter should (and should not) be conducted! If you have never seen or participated in a telehealth encounter, we would strongly recommend running through these very real life situations. In addition, download the following which has several very practical checklists:
Additionally, here are two checklists on telehealth etiquette that you might find useful. We recommend printing one of these out and having it with you as you get started with telehealth visits. Take notes and add/adapt it as you discover new lessons learned!
-
- Telehealth Etiquette Checklist.
- Telehealth Visit Etiquette Checklist (American Medical Association)
- What about telephone etiquette? The American Academy of Family Physicians has developed two good resources for those conducting telephone visits:
Clinical Assessment and the Physical Exam
- Are there any practice guidelines for providing clinical care using telehealth?
- The American Telemedicine Association (ATA) has developed Practice Guidelines for Live, On Demand Primary and Urgent Care.
-
- Depending on the type of provider you are and the type of service you offer, there are other specific clinical guidelines and best practices for telehealth that have been developed. The ATA has some of these other practice guidelines in their Practice Guidelines Archive.
-
- In response to the pandemic, Harvard Medical School is waiving tuition for their online course on The Telephone & Telemedicine in Clinical Medicine: An Instrument of Opportunity & Risk (includes 3 AMA PRA Category 1 Credits).
- How do I perform a physical exam by telehealth? Following are some great resources to help you with this!
- This article "Why the Telemedicine Physical is Better than You Think" gives some great perspective as well as some very practical ideas about what can be done even without peripheral devices.
-
- ODU's Center for Telehealth Innovation, Education and Research (C-TIER) has developed Telehealth training videos. The focus of this series is on physical exams via Telehealth. Several of these videos show how practitioners instruct the patient in a self-exam with the use of a tablet and/or computer, along with a series of questions. Other videos in this series show how practitioners can use various Telehealth devices to conduct physical exams and consult with specialists.
- Telehealth Physical Exam: ENT
- ODU's Center for Telehealth Innovation, Education and Research (C-TIER) has developed Telehealth training videos. The focus of this series is on physical exams via Telehealth. Several of these videos show how practitioners instruct the patient in a self-exam with the use of a tablet and/or computer, along with a series of questions. Other videos in this series show how practitioners can use various Telehealth devices to conduct physical exams and consult with specialists.
-
-
- Telehealth Physical Exam: Skin
-
-
-
- Telehealth Physical Exam: Abdominal
-
-
-
- Telehealth Physical Exam: Cardiopulmonary
-
-
-
- Telehealth Physical Exam: Neurological
-
-
-
- Telehealth Physical Exam: Musculoskeletal
-
-
-
- Introduction to Conducting Physical Exams via Telehealth with Devices
-
-
-
- Conducting a Pediatric Well-visit using a Mobile Telehealth Device
-
-
-
- Using Remote Patient Monitoring (RPM) Equipment to Assess Congestive Heart Failure
-
-
-
- Mobile Telehealth Device used to Assess Back Pain between Nurse Practitioner and Specialist
-
-
-
- Telehealth Robot Assists Nursing Facility Staff Communicate Assessment with Primary Care Provider
-
-
-
- Pre-op Airway Assessment via a Telehealth Cart and Oral Camera
-
-
- If you want to kill two birds with one stone, this is an excellent online training developed by Thomas Jefferson University Sidney Kimmel Medical College on Telemedicine: Conducting an Effective Physical Exam Online Course ($100 for this 1 hour online course that includes CME/CE)
-
- CaravanHealth has developed detailed guidance on the Telehealth Physical Exam as well as detailed guidance on Adapting the Annual Wellness Visit to Telehealth
-
- The American Academy of Ophthalmology has developed this guidance on the Home Eye Test for Children and Adults. This website guidance page also includes downloadable home eye testing charts.
- What if I am using the telephone?
- The CDC has developed Phone Advice Line Tools: Guidelines for Children or Adults with Possible COVID-19. This document includes initial phone scripts, accompanying decision algorithm and tailored care advice messages.
-
- In response to the pandemic, Harvard Medical School is waiving tuition for their online course on The Telephone & Telemedicine in Clinical Medicine: An Instrument of Opportunity & Risk (includes 3 AMA PRA Category 1 Credits).
Meeting the Needs of Patients/Clients Who Need Interpreters or Have Disabilities
- Section 504 of the Rehabilitation Act of 1973 – applies to federal health care services and facilities; and health care providers who are also recipients of federal financial assistance, usually provided by direct funding (such as federal Medicaid funds) or by grants (such as a federal research grant).
- Title II of the Americans with Disabilities Act – applies to all public (state and local) health care providers.
- Title III of the Americans with Disabilities Act – applies to all private health care providers.
- Things to consider when weighing your options:
- Video interpretation, when possible, will be a better option than audio only because the majority of communication is done nonverbally!
- A trained healthcare interpreter will almost always be better than using staff, family or friends. Some patients will insist on using family members or friends. Don't be afraid to offer an alternative if you have one.
- Here are a few resources you may want to review:
- If you have access to a trained healthcare interpreter:
- There are many videoconference platforms that allow for multi-point videoconferencing. There is no reason not to continue to use your interpreter remotely by video.
- As an example, Zoom for Healthcare has a built-in feature that allows you to add an interpreter as well as a closed captioning and live transcription. While Zoom has a pilot integration with otter.ai for artificial intelligence driven transcription, it is not recommended for important healthcare communications due to the often technical vocabulary being used. If you do use this feature, please monitor and correct errors continuously and carefully. To find a Communication Access Realtime Translation (CART) provider (real-time captioning or live-event captioning), please visit the National Court Reporter's Association Sourcebook and search for CART Captioning services.
- There are many videoconference platforms that allow for multi-point videoconferencing. There is no reason not to continue to use your interpreter remotely by video.
- If you don't have access to a trained healthcare interpreter:
- The National Board of Certification for Medical Interpreters has a searchable registry of interpreter training programs. These programs may be able to direct you to certified medical interpreters in your state. These individuals may or may not have had training in video/remote interpretation.
- There are some telehealth platforms that have integration of healthcare interpreter services (both language and AS:L) as part of their license agreement with end-users.
- Examples of such platforms include ViTelNet and Cloudbreak
- There are remote interpretation companies that provide interpretation by video.
- Examples of such companies include Stratus Video/InDemand Interpreting and LanguageLine Solutions. You will likely find many others with a simple search. Make sure you ask for someone who is trained in healthcare interpretation. .
- Do not use Google Translate for important healthcare communications. Google Translate has only 57.7% accuracy when used for medical phrase translation! If you have no other options and can't reschedule the visit at a time when an interpreter is available, a somewhat better alternative would be the Instant Language Assistant app being made temporarily available to providers for free during the pandemic.
- If you are an interpreter or know one that has never done interpretation by video before:
- Please take a look at our Telehealth Etiquette video resources found in our section on Best Practices for Conducting a Telehealth Visit in this COVID-19 Resource toolkit..
- The National Council on Interpreting in Health Care has a number of good resources, including these two webinars:
- Temporary Transition to Remote Interpreting During Health Emergencies: Guidance and Tips for Language Access Stakeholders (recorded webinar is free for NCIHC members and $30 for non-members, but slides and FAQs may be accessed for free by all)
- The Critical Role of Healthcare Interpreters During the COVID-19 Pandemic: Legal and Practical Implications (free live webinar on April 25, recording will be free for NCIHC members and at cost for non-members)
- How do I help my non-English speaking patients understand and prepare for a telehealth visit?
- In response to the increased use and expanded coverage of telehealth during the COVID-19 pandemic, From Coverage to Care (C2C) has released new resources to support patients and providers in making the most of virtual care. They have developed a guide called Telehealth: What to Know for Your Family. It is available in eight languages: English (PDF), Arabic / ال عرب ية (PDF), Chinese / 中文 (PDF), Haitian Creole / Kreyòl Ayisyen (PDF), Korean / 한국어 (PDF), Russian / Русский (PDF), Spanish / Español (PDF), Vietnamese / TIẾNG VIỆT (PDF)
- How do I help my non-English speaking patients navigate technology?
- What are the specific considerations for patients/clients with disabilities? Here is a nice graphic developed by the Northwest Regional TRC that answers this question:
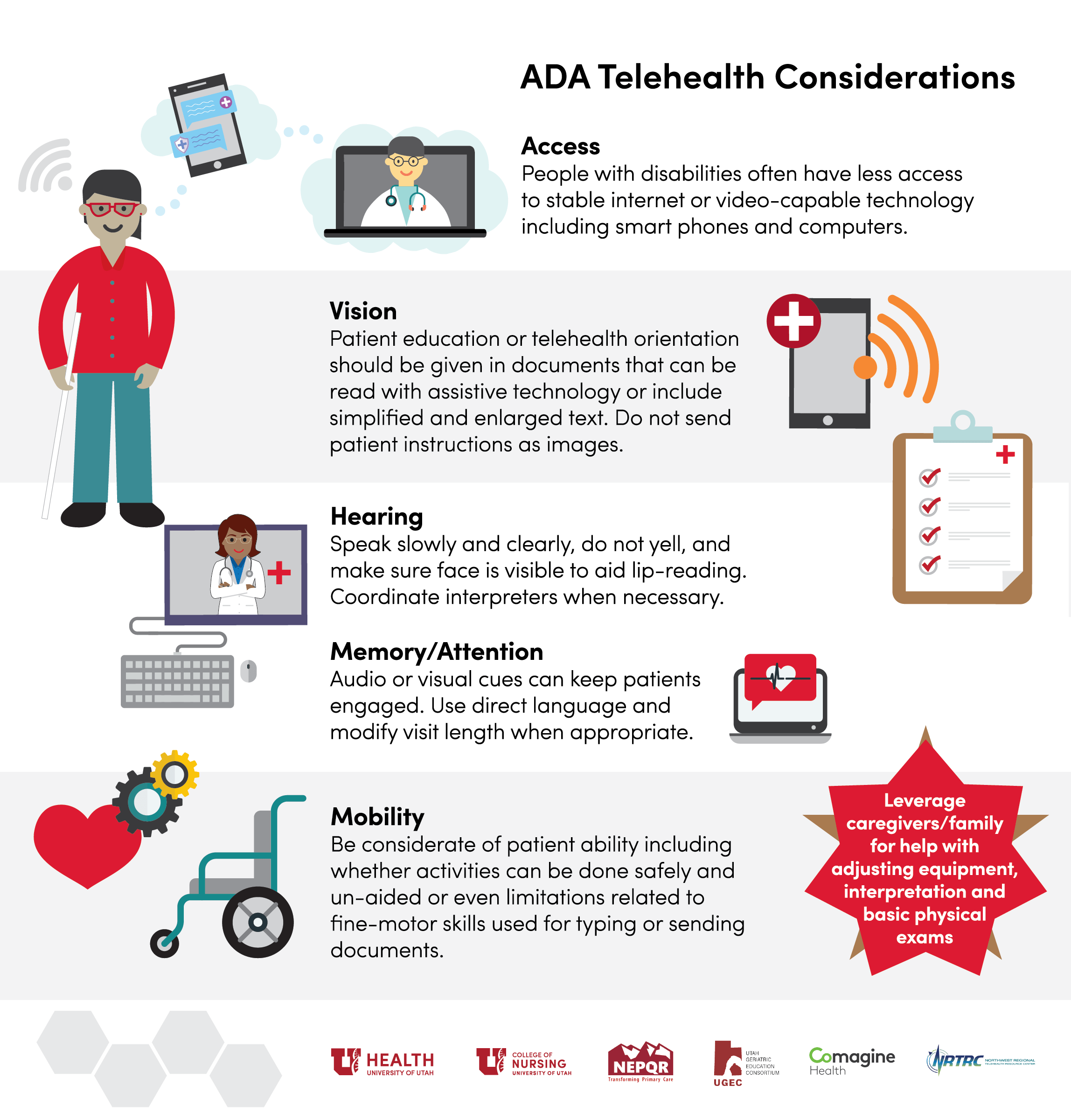
- What kind of auxiliary aids and services are required by the ADA to ensure effective communication with individuals with hearing or vision impairments?
- The ADA National Network has compiled a really nice list of appropriate auxiliary aids and services.
- What if I have a deaf or hard of hearing patient? The options mentioned above for language services would also apply to interpretation for those who are deaf or hard of hearing, including most, if not all of the examples of platform and interpretation service providers/vendors. Additionally, below are some specific best practice for this population with special needs:
- The National Association of the Deaf has developed the following resources:
-
- Hearing Loss Association of America has developed the following resources:
-
- The North Carolina Department of Health and Human Services has created several excellent telehealth guidance documents for Healthcare Providers:
-
- If you are an ASL interpreter, the Southwest Telehealth Resource Center hosted this webinar on ASL Interpreters (on video or in person) in Medical Settings and the Law that might be of interest. Although some of the materials are specific to Arizona, much of it is relevant to all ASL interpreters.
-
- Free sign language is being offered by Virtual Remote Interpretation by linguabee for COVID-19 test sites during the pandemic.
-
- iCanConnect, also known as the National Deaf-Blind Equipment Distribution Program (NDBEDP), was established by the Federal Communications Commission (FCC). iCanConnect provides free equipment including smartphones, tablets, computers, screen readers, braille displays, and more to people who meet federal disability and income guidelines.
-
- National Assistive Technology Act Technical Assistance and Training (AT3) Center is your one-stop connection to information about the Assistive Technology Act, State Assistive Technology Programs, and general assistive technology and has this Program Directory of State Assistive Technology Programs.
Educating the Patient About Telehealth
- What can I give or share with my patients/clients to help them understand telehealth?
- Here are a few infographics and patient resources that can help patients better understand what a telehealth visit
-
-
- How Patients Can Engage Telehealth:
-
-
-
- Telebehavioral Health (this was created by the Upper Midwest TRC and provides a brief overview of Telebehavioral Health)
-
- Do you have a script for me to use to explain telehealth and virtual care to my patients/clients?
- The South Central TRC has developed this tip sheet: How to Engage Your Patients in Telemedicine
-
- CaravanHealth has developed these two templates that you can use to help you communicate with your patients about telehealth and other types of virtual visits:
- How do I help my patients/clients understand about the need for an internet connection and learn about the technology needed for a telehealth visit?
- Family Voices received 2020 CARES Act funds to support telehealth for families of children with Special Health Care Needs. Many of these resources are broadly applicable to all families.
- "Are You Connected Webinar" to help families with children with special health care needs to understand the basics about getting and improving their cellular or WiFi connection. They have also developed the following infographics for addressing common barriers to connectivity:
- Family Voices received 2020 CARES Act funds to support telehealth for families of children with Special Health Care Needs. Many of these resources are broadly applicable to all families.
-
-
- "Do You Have a Device Webinar" to help families with children with special health care needs to understand that computers, laptops, tablets and smartphones can all be used for a telehealth visit and to learn if their device is "teleready". They have also developed the following infographic:
-
-
-
- "Can You 'See' Your Provider Webinar" to help families learn the keys for a successful family centered telehealth appointment. They have also developed the following infographics:
-
-
- Telehealth Access for Seniors has developed a large number of easy to understand downloadable Tech Guides that may be useful. Their website includes guides for Gmail Setup, Wifi, MyChart App, MyChart Website, Apple-ID Setup, Android Device, Amazon Fire and Play Store. There are also several guides in Spanish, Korean, Chinese and Arabic.
- How can I help my patient/client be prepared for a telehealth visit?
-
- Here is an outstanding video for patients developed by the State of Hawaii Department of Health Genomics Section and Western States Regional Genetics Network (UH7MC30774-01-00) in collaboration with the Pacific Basin Telehealth Resource Center to help patients understand telehealth, what to expect and how to prepare.
-
- We (MATRC) wrote this article on How to Help a Family Member or Friend with Their First Telehealth Visit for Senior Navigator.
-
- In response to the increased use and expanded coverage of telehealth during the COVID-19 pandemic, From Coverage to Care (C2C) has released new resources to support patients and providers in making the most of virtual care. They have developed a guide called Telehealth: What to Know for Your Family. It is available in eight languages:
-
- The California Telehealth Resource Center has developed this Infographic: How Do I Use Telehealth? Frequently Asked Questions and Insights for Patients
-
- Doctors Technology Office has developed this Virtual Care Frequently Asked Questions for patients to prepared them for a visit along with troubleshooting tips.
-
- The American Psychiatric Association and SAMHSA has developed this infographic on How to Prepare for a Video Appointment with Your Mental Health Clinician.
-
- The Center of Excellence for Protected Health Information through funding by SAMHSA has developed this Infographic on Tips to Keep Your Telehealth Visit Private. This has some very practical advice for patients/clients related to protecting communications, creating the right environment and protecting their devices.
-
- The South Central TRC has created this infographic on Make the Most of Your Telemedicine Visit: For Patients. This easy to follow three-pager providers an excellent overview for patients on what is telehealth, why use telehealth, what to expect from a visit and how to prepare for a visit.
-
- The Upper Midwest TRC has created this infographic about Your Telemedicine Appointment. This easy to understand one-pager providers an excellent overview for patients on how to prepare for an appointment.
-
- All in for Health and The Children's Partnership have developed this Fact Sheet on Telehealth + Children: Frequently Asked Questions
-
- Family Voices has developed "Your Family's First Telemedicine Appointment Webinar" to help families of children with Special Health Care Needs prepare for a successful family centered telehealth visit. They have also developed the following infographics:
Specialty and Setting Specific Guidance Documents
- Here you will find links to medical and advanced practice nursing specialty specific guidance developed by different professional associations/organizations:
- The American Academy of Dermatology has developed this Teledermatology Toolkit
-
- The American Academy of Neurology has put together the following resources:
- Telemedicine and COVID-19 Implementation Guide
- Telemedicine and COVID-19 FAQ
- NeuroBytes: The Neurologic Exam Via Telemedicine training course that is free to AAN members
- NeuroLearn: Introduction to Teleneurology training course that is free to AAN members and for a fee for nonmembers that includes 1.0 CMEs..
- The American Academy of Neurology has put together the following resources:
-
- The American Academy of Pediatrics has provided a number of Sample Documents, including a Telehealth Visit Protocol, Patient Recruitment Sample Letter, Swimlane Workflows and Start-up Checklist for Connecting a Specialist to a Private Practice. In addition, they have developed this webinar on Telehealth and COVID-19.
-
- The American Association of Nurse Practitioners has developed this training on Telehealth: What Nurse Practitioners Need to Know that is free to AANP members and for a fee for nonmembers that includes CE Credits.
-
- The American College of Cardiology put together this podcast: Practice Made Perfect: Telehealth Ensuring Quality Cardiovascular Care During Uncertain Times.
-
- The American College of Physicians has developed An ACP Physician's Guide that has a section on telehealth, has developed a curriculum called Telemedicine: A Practical Guide for Incorporation into your Practice and has put together this webinar on Revving Up Your Telemedicine Practice in the Time of COVID.
-
- The American Diabetes Association has developed this webinar on Telehealth and COVID-19
-
- The American Medical Association has developed a "Quick Guide to Telemedicine in Practice" that has a section on Practice Implementation.
-
- The American Society of Cataract and Refractive Surgery has developed this webinar on Implementing Tele-Ophthalmology During COVID-19 Pandemic
-
- The American Urological Association has put together this white paper on Telemedicine in Urology as well as a number of other valuable resources in their Telemedicine Info Center for COVID-19.
-
- The Association of Community Cancer Centers has developed a resource page on Coronavirus Response for Cancer Care.
-
- The Federal Interagency Committee on EMS has developed this Telemedicine Framework for EMS and 911 Organizations.
-
- The National Rural Health Resource Center partnered with the Northwest Regional Telehealth Resource Center to develop this Critical Access Hospital Telehealth Guide.
-
- The Providers Clinical Support System (PCSS) has developed FAQs for Treating Opioid Use Disorder via Telehealth Tips for Primary Care Providers
-
- The Society of Critical Care Medicine has developed this "Tip Sheet: Application of Telemedicine and Telecritical Care to Emergency Management of COVID-19
Teledentistry
- What is exactly teledentistry and how will this help me during COVID-19 and Beyond?
- Check out these these resources for a nice overview!
- American TeleDentistry Association Facts About Teledentistry
- CareQuest Institute for Oral Health:
- Teledentisty: What to Know & How It Works
- Teledentistry: Providing Access to Care During the Covid-19 Crisis
- Using Teledentistry to Maintain Services and Contact with Patients During COVID-19
- Approaches for Prioritizing Care in Response to COVID-19
- Expanding Oral Health: Teledentistry
- Teledentistry Use Beyond the Pandemic
- Check out these these resources for a nice overview!
-
- Now take a look at this webinar by Dr. Paul Glassman on Teledentistry and Minimally Invasive Procedures in the Time of COVID-19:
- How do I get started?
- The National Network for Oral Health Access (NNOHA) has developed this Teledentistry Learning Collaborative Teledentistry User Guide.
-
- Virginia Health Catalyst has developed these very practical tools along with the following video showing a practice teledentistry visit for dentists getting started::
- American Teledentistry Association Guidelines for Teledental Practice
- Crisis Teledentistry Implementation Guide (a few of the pages are specific to Virginia policies, but but the rest of the document has great information about teledentistry practice recommendations and resources)
- Teledentistry Workflow Chart
- Practice Teledentistry Visit Video:
- Virginia Health Catalyst has developed these very practical tools along with the following video showing a practice teledentistry visit for dentists getting started::
-
- Teledent has put together this guidance document on Patient Assessment via Synchronous Teledentistry
-
- The American Dental Association (ADA) has put together this Guide to Understanding and Documenting Teledentistry Events.
-
- CareQuest Institute for Oral Health has put together this great teledentistry etiquette video on Answering that Dental Emergency Call Remotely:
- The American Teledentistry Association has put together this Industry Standards for Remote Orthodontic Treatment
- CareQuest Institute for Oral Health has developed some very nice resources for providers to give to their patients:
Telegenetics
Here are some additional resources that you might find useful as well:
- The National Coordinating Center for the Regional Genetics Networks has a Telemedicine/Telehealth Resource Page that has a great resource repository.
- The National Genetics Education and Family Support Center has developed a patient facing infographic called TELEWHAT?: An Introduction to Telegenetics that might be useful for you or provide your patients..
Telehealth and Autism Care
- The Council of Autism Service Providers has developed a number of resources:
- Practice Parameters for Telehealth-Implementation of Applied Behavior Analysis
- Organizational Guidelines & Standards
- Webinar on Autism Telehealth in Crises and Beyond
- Webinar Video (free but registration required)
- Webinar Slides
- Behaviorbabe has a great website on ABA and Telehealth. Following is video about ABA, Telehealth and COVID19 from their website (many more videos and other resources on the website as well):
- There is a Telehealth in ABA Facebook Group with some great ideas. It is a private group so you will need to request to join.
- The Behavioral Health Center of Excellence has developed the following webinars to assist providers:
- K-Now Solutions has put together this webinar on Telehealth in ABA: The Building Blocks
- Psych Central has this reflection post on Tele-ABA Activities for Kids: 7 Telehealth Activities ABA Providers Can Use with Children with ASD
- Insight + Regroup is offering this online 1 CME credit training course on Telepsychiatry and Children with Autism Spectrum Disorder free of charge during the pandemic.
- Professionals in Italy developed this paper on a Model of Support for Families of Children with Autism Living in the COVID-19
- This is an excellent blog post on 10 Strategies for Engaging Parents (not Children?) during Tele-Intervention
- MSU Autism Lab hosted this webinar on Parent Coaching through Telehealth:
- Behavior Development Solutions has developed a course on Coaching Caregivers Through the Internet; Challenges and Solutions for Successful Telehealth Services. There is a small fee for the course, but 1.5 BACB Learning CE credits are being offered.
- Family Voices received 2020 CARES Act funds to develop a host of resources to support telehealth for families of children with Special Health Care Needs. Visit their website to see training resources, toolkits and more. Many of these resources are detailed in our section on Educating the Patient About Telehealth.
You may also want to visit our section of resources on Telerehabilitation, Telepractice and Early Intervention Services!
Telehealth for Post-Acute and Long-Term Care Settings and Services
- West Health, in partnership with the AARP and the National Consortium of Telehealth Resource Centers has put together this webinar on The Use of Telehealth in Long Term Care Settings During this National Emergency (click here for Powerpoint slides)
- West Health has also developed a number of resources for PALTC settings:
- Getting Started with Telehealth: PALTC
- Getting Started with Telehealth: Provider (with PALTC)
- A Practical Guide to Telehealth: Implementing Telehealth in Post-Acute and Long-Term Care Settings (PALTC)
- Rapid Deployment: Getting Started with Telehealth Pre-visit Form: PALTC
- Rapid Deployment: Getting Started with Teleheallth Post-visit From: PALTC
- Telehealth Workflow for Post-Acute and Long Term Care Facilities
- The Society for Post-Acute and Long-Term Care Medicine has published Standards for the Use of Telemedicine for Evaluation and Management of Resident Change of Condition in the Nursing Home
- The American Psychological Association has put together How to Provide Telehealth in Nursing Homes, with tips for offering essential psychological services to older residents during the pandemic.
- Altarum recently released a report entitled Rapid PACE Responses in a Covid-19 Era: How PACE Providers Have Innovated and Adapted to Keep Enrollees Safe in Their Communities.
- LeadingAge has developed a number of guides for the selection and implementing of technologies:
- Telehealth and Remote Patient Monitoring for Long-Term and Post-Acute Care: A Primer and Provider Selection Guide
- Social Connectedness and Engagement Technology for Long-Term and Post-Acute Care: A Primer and Provider Selection Guide
- Safety Technology for Long-Term and Post-Acute Care: A Primer and Provider Selection Guide
- Medication Management Technologies for Long-Term and Post-Acute Care
- Electronic Health Records (EHRs) for Long-Term and Post-Acute Care: A Primer on Planning and Vendor Selection
- Functional Assessment and Activity Monitoring Technology: A Primer and Provider Selection Guide
- Shared Care Planning and Coordination Technology for Long Term and Post-Acute Care: A Primer and Provider Selection Guide
- Resident/Client Technology Support and Training Guide
Telehospice and Telepalliative Care
- The Center to Advance Palliative Care has put together a comprehensive Telehealth and Palliative Care Toolkit with both downloadable guidance documents and web-based resources in the following areas:
- Setting Up a Program
- Preparing Patients and Families
- Conducting Telehealth Visits: Etiquette
- Conducting Telehealth Visits: Remote Physical Examination
- Telehealth Documentation and Billing
- The Journal of Palliative Medicine as published an article on Top Ten Tips Palliative Care Clinicians Should Know About Telepalliative Care
- The National Hospice and Palliative Care Organization (NHPCO) has put together a number of excellent resources:
- The Shiley Haynes Institute for Palliative Care has put together a 4 hour self-paced online course that includes 4 CE/CME Credits on Telemedicine Skills for Clinicians. Total cost of the course is $79.In addition, they have made available the following recorded Six Session Telemedicine Now (and How!) Connecting at a Distance Open Forum Series:
-
- Session 1: Effectiveness and Connection via Telemedicine: Getting Past the (Real and Imagined) Hurdles
-
- Session 2: Expert Q&A on Symptom Management and Patient Education at a Distance
-
- Session 3: Virtually Anything in COVID-19: The Many Uses of Technology for Caring
-
- Session 4: Best Practices for Hosting Sensitive Conversations by Video
-
- Session 5: Boundaries and Intimacy: How Deeply Can We Connect at a Distance?
-
- Session 6: Emergency Medicine, Nursing Home Residents, and Tele-Palliative Care: Past, Present, and Future
- :The National Care Planning Council has put together About Telehospice Care as part of their Guide to Long Term Care Planning.
- Husch Blackwell has developed this Hospice Telehealth Flowchart: How to Provide Medically Necessary Hospice Physician and Nurse Practitioner Visits via Telehealth to Medicare Hospice Patients During the COVID-19 Pandemic
- The Association of Professional Chaplains has developed is A Quick Guide to Providing Telechaplaincy Services
Telerehabilitation, Telepractice and Early Intervention Services
- Physical Therapy:
- The American Physical Therapy Association has put together a number of telehealth resources. Here is just a sampling:
-
- The Federation of State Boards of Physical Therapy Guidelines: Telehealth in Physical Therapy
-
- The Family, Infant and Preschool Program has put together this infographic for Physical Therapists on Tele-Move: I'm a PT, Don't Take My Hands Away From Me
-
- The Inspired Treehouse has some great and mostly free child development resources for parents and professionals, including a set of digital therapy games. Many of the free resources can be used virtually.
-
- There are a few vendors that have developed some technology based solutions for Physical Therapy applications that may be of interest to some.
Please note that MATRC is not in a position to either endorse or recommend any of the above vendors. We strongly encourage you to do your due diligence when making a vendor selection. There may be other vendors with a PT specific focus, these are simply ones that have been brought to our attention thus far.
- Occupational Therapy:
- The American Occupational Therapy Association has put together a number of telehealth resources. Here is just a sampling:
-
- The American Congress of Rehabilitation Medicine as put together this webinar on Telehealth Resources for Occupational Therapy
-
- OTPotential has developed this informative Telehealth Occupational Therapy Guide that you might also find useful.
-
- The Family, Infant and Preschool Program has put together this infographic for Occupational Therapists on Tele-Sense: Making Sense of Sensory Preferences
- Telepractice/Telespeech:
- The American Speech-Language-Hearing Association (ASHA) has put together a number of resources on telepractice. Here is just a sampling:
-
- We have a recorded webinar on "Innovation and Impact with Speech Language Pathology Telepractice
-
- SpeechPathology.com offers a two-part course on Pediatric Telepractice with CEUs for $99/year: Telepractice: What You Need to Know for Practical Applications in Pediatrics and Telepractice: Day in the Life of a Teletherapist, the Inside Scoop
-
- Pearson Assessments provides a brief How To on Telepractice and a video demo of Q-global Quick Look Demo for Speech Language Pathologists for conducting the CELF-5 and GFTA Assessments.
-
- The Family, Infant and Preschool Program has put together this infographic on Tele-Speech: SLPs, Can We Talk? Our Virtual Role
- Early Intervention Services (you may also want to visit our earlier section of resources on Telehealth and Autism Care):
- The Family, Infant and Preschool Program (FIPP) has put together an amazing set of resources on Early Childhood Intervention Telepractice, including a set of Tele-Practie Infographics and this video on Providing Early Intervention Services Through Distance Technology:
-
- The Infant and Toddler Connection of Virginia put together this Teleflections Video Series which provides reflections from Virginia early intervention service providers on tele-intervention:
- Teleflections Video 1 – My First Online Visit
- Teleflections Video 2 – Tele-What?!
- Teleflections Video 3 - Bandwidths, Platforms, and Pings?? Help!
- Teleflections Video 4 - I'm a PT and Rely on my Hands
- Teleflections Video 5 – Woke Up Worried
- Teleflections Video 6 - Mom was Over the Moon
- Teleflections Video 7 - Update from Julie
- Teleflections Video 8: Getting Creative in Rural Areas
- The Infant and Toddler Connection of Virginia put together this Teleflections Video Series which provides reflections from Virginia early intervention service providers on tele-intervention:
They also hosted this webinar on Telepractice in Early Intervention:
-
- This document has some very practical information on Planning for the Use of Video Conferencing for Early Intervention Home Visits during the COVID-19 Pandemic
-
- ASHA offers several resources on early intervention services. These include:
- Using Telepractice to Provide Early Intervention Services to Families
- Online Conference Session (free to members) on The State of Telepractice for Delivering Early Intervention Services
- ASHA offers several resources on early intervention services. These include:
-
- Sweet Pea Pediatric Wellness has made available this video on Getting Started with Telehealth for Early Intervention Providers - Tips & Tricks
-
- The Early Childhood Technical Assistance Center has put together a presentation on Use of Tele-Intervention in Early Intervention (IDEA Part C): Strategies for Providing Services Under the COVID-19 Public Health Emergency
-
- The National Center for Hearing Assessment and Management has put together A Practical Guide to the Use of Tele-Intervention in Providing Early Intervention Services to Infants and Toddlers Who Are Deaf or Hard of Hearing
-
- Family Voices received 2020 CARES Act funds to develop a host of resources to support telehealth for families of children with Special Health Care Needs. Visit their website to see training resources, toolkits and more. Many of these resources are detailed in our section on Educating the Patient About Telehealth as well as our section on Best Practices for Conducting a Telehealth Visit, subsection on "What Should I Do If My Patient/Client Needs an Interpreter"
- Telehealth Technology specific to telerehabilitation for Speech, OT, PT, ABA and more are available and can make help facilitate care. While MATRC cannot endorse or recommend any particular vendors, below is just a sampling of a few things available in the market.
*Please exercise due diligence whenever making decisions about technologies and vendors. Consult with our Vendor Selection Toolkit and take advantage of our Virtual Office Hours related to Technology and Vendors if you need some assistance navigating the technology and vendor space!
Tele-Substance Use Disorder Treatment and Recovery Services
- View our conference session on Behavioral Health and Substance Use Disorder: Telehealth Implementation and Practice Considerations: This session will help you understand how a behavioral health organization quickly implemented telehealth practices during COVID-19 and address billing and coding, approaches to inpatient and outpatient care, explore differences between telephonic and video telehealth and identify innovative ways to adjust workflows to meet patient needs.
- The Addiction Technology Transfer Center (ATTC) Network, funded by SAMHSA has developed the following resources:
-
- Telehealth Learning Series for SUD Tx and Recovery Support Providers (live one-hour sessions each week with access to experienced providers, training tools, checklists and more). There is an archive of recorded past session materials.
- SBIRTcolorado.org has developed this outstanding guidance document on Screening, Brief Intervention, Referral to Treatment (SBIRT & Telehealth)
- We have, as part of our Telebehavioral Health Center of Excellence website, a page of general MAT and Tele-MAT Resources
- The Providers Clinical Support System (PCSS) has developed FAQs for Treating Opioid Use Disorder via Telehealth Tips for Primary Care Providers
- The DEA has provided this Policy Guidance documents:
- The Center of Excellence for Protected Health Information has developed this slideset from a webinar on Understanding the New SAMHSA/OCR Guidance for Telehealth SUD and MH Services
- The National Council for Behavioral Health made available this recorded COVID-19 Office Hour session focused on Opportunities for Peer Support Workers, Supervisors and Programs
- The Center for Connected Health Policy has put together this report on Barriers & Challenges to FQHC Use of Telehealth for Substance Use Disorder: A Examination of Policies Affecting FQHCs Pre- and During COVID-19 Emergency.
- The Substance Abuse and Mental Health Services Administration (SAMHSA) as part of their Evidence-Based Resource Guide Series has developed Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders
Impact of COVID-19 on Federal and State Policies
- For a summary the array of policy changes as a result of the pandemic, visit: COVID-19 Telehealth Coverage Policies
- For more information, including a searchable database by topic and by state, visit Telehealth in the Time of COVID-19.
- If you are a licensed psychologist, the American Psychological association has also tracked State Actions Relevant to Licensed Psychologists During COVID-19.
- The US Health and Human Services must officially renew the public health emergency (PHE), a status that allows many of the waivers and expansions for telehealth that have occurred since the COVID-19 pandemic began in March 2020 to remain active. Each renewal extends the PHE an additional 90 days. The latest renewal, which occurred on April 13, 2022 extends the PHE through July 11, 2022.
Licensure, Interstate Practice and Credentialing/Privileging
- Licensure Exemptions Under the 4th Amendment to the Declaration under the PREP Act- Medical Countermeasures Against COVID-19. On December 3, 2020, the US Department of Health and Human Services (HHS) issued a fourth amendment to the Declaration Under the Public Readiness and Emergency Preparedness Act (PREP Act) for Medical Countermeasures Against COVID-19. In the amendment was the inclusion of a telehealth provider under the “covered person” designation. The amendment further noted that if a telehealth provider was delivering a “covered countermeasure” via telehealth to a patient in a state the telehealth provider was not licensed it, state laws, including state licensure requirements, that prohibited such actions would be pre-empted. A telehealth provider who is not licensed in the state the patient is located in, will be able to provide a select set of services without having to be licensed. However, there are certain qualifications and parameters that must be met. Read this Fact Sheet to better understand which situations would allow for licensure exemption.
- Patients/Clients From Multiple States See Me In My Office. May I Continue to See Them Using Telehealth During This Pandemic? In general, a clinician must be licensed in the state where the patient/client is physically located at the time of service. Former President Trump declared an emergency on March 13, 2020. As a result, the Centers for Medicare & Medicaid Services (CMS) has authorized the 1135 Waiver that took effect retroactively to March 1, 2020. This waiver is limited in scope to conditions of participation and payment for Federal health care programs such as Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP). Authorization of this waiver alone DOES NOT waive the requirement for physicians and other healthcare providers to maintain licensure in states where they are practicing a licensed profession, including via telehealth. What the waiver does is that it gives States the option of being able to do so. State law continues to govern whether a provider is authorized to provide professional services in that state without holding an active license from that state’s medical board. Many state medical and other health professions licensing boards have created mechanisms that either waive or expedite state licensure requirements in response to the pandemic.
- We Work with College or University Students and They Are Now Dispersed Throughout the Country. May I Continue to See Them or Assist Them? As mentioned earlier, in general, a clinician must be licensed in the state where the patient/client is physically located at the time of service. However, in conversations with multiple state licensing boards, most provide leniency around this when it comes to pre-existing relationships and continuity of care. Additionally, many state medical and other health professions licensing boards have created mechanisms that either waive or expedite state licensure requirements in response to the pandemic. If the state where your student is has not already made provisions for interstate practice during the pandemic, I would recommend contacting the licensing board for your health profession and just verifying that they will be OK with going across state lines to maintain continuity of care for a college student.
- On April 15, 2020, student representatives from over 130 universities across the country signed onto a Letter Addressed to the State Medical Licensing Boards for Mental Health Providers encouraging them to mandate an update on interstate licensing requirements so that mental health care providers can meet the needs of their students who happen to be residing in different states as a result of COVID-19. This is a developing issue that we will be monitoring.
- We work with a variety of non-physician health care practitioners. What do I need to consider when thinking about interstate telehealth practice? As mentioned earlier, in general, a clinician must be licensed in the state where the patient/client is physically located at the time of service. In additional to understanding the telehealth specific laws and rules in each state, there are a few other policy considerations that need to be researched and understood. A few of these include:
-
- Scope of practice laws: Each state has different policies related to Scope of Practice for different types of providers. If a practitioner is licensed in multiple states and is using telehealth to provide services across state lines, that practitioner needs to keep in mind what he/she may or may not do based on the laws of the state where the patient/client is located at the time of service. The NCSL Scope of Practice Policy website provides good information about Behavioral Health Providers, Nurse Practitioners, Oral Health Providers, Pharmacists and Physician Assistants by state. Please note that providers for some professions and in some states are required to have collaborative practice agreements with a physician. In this case, the collaborating physician must also be licensed in the State where the patient is physically located at the time of service.
- Malpractice coverage: The provider/practitioner (and collaborating physician if one is required) needs to check with their malpractice carrier to make sure they are covered for both telemedicine services (most do, but some require an additional rider) and that the coverage extends beyond state lines. Additionally, if it does extend beyond state lines, they also need to make sure that the malpractice coverage cap (or no cap) aligns with the different state’s malpractice policies. Different states have caps in widely varying amounts and others don’t have caps at all. The coverage needs to be adequate to meet all the different state requirements.
-
- Which state medical and other health professions licensing boards have created mechanisms that either waive or expedite state licensure requirements in response to the pandemic? Here are several professional organizations and associations that have been tracking changes to telehealth licensure policy during the pandemic:
-
- The Multi-Discipline Licensure Resource Project has been developed to serve as an information hub for Occupational Therapists, Physical Therapists, Psychologists and Social Workers
-
- Telemental Health Training Institute States' Rules and Regulations has a database by topic, including States' Responses to COVID-19. Specific for counselors, social workers, marriage and family therapists and psychologists.
- I hear that some states participate in interstate compacts for practitioners. Can you tell me more about those? As interstate practice through telehealth has expanded, many professions and states have developed efforts to facilitate interstate practice. The following are the compacts that have been developed (or are in process of being developed).
- APRN Compact: The APRN Compact allows an advanced practice registered nurse to hold one multistate license with a privilege to practice in other compact states. This compact has been adopted, but has not yet been implemented. It will be implemented once 7 states have enacted legislation for joining the compact.
- Audiology & Speech-Language Pathology Interstate Compact (ASLP-IC): The ASLP-IC facilitates the interstate practice of audiology and speech-language pathology while maintaining public protection.
- EMS Compact: The EMS Compact facilitates the day to day movement of EMS personnel across state boundaries in the performance of their EMS duties as assigned by an appropriate authority. The EMS Compact authorizes state EMS offices to afford immediate legal recognition to EMS personnel licensed in any other member state.
- Interstate Medical Licensure Compact (IMLC): The Interstate Medical Licensure Compact offers a voluntary, expedited pathway to licensure for qualified physicians who wish to practice in multiple states. Please note that this is not the same as reciprocity between participating states. Some states who do not participate in the Compact have a process called "Licensure by Endorsement" that also creates a more efficient/expedited process for a physician who is licensed and in good standing in one state to get licensed in another state.
- Nurse Licensure Compact (NLC) The Nurse Licensure Compact allows a nurse to have a multistate license with the ability to practice in their home state and all participating compact states. This is considered reciprocity between participating states.
- Psychology Interjurisdictional Compact (PSYPACT): PSYPACT is designed to facilitate the practice of telepsychology and the temporary in-person, face-to-face practice of psychology across state boundaries.
- Physical Therapy Compact (PT Compact): The PT Compact is an agreement between participating states that allows PTs and PTAs more mobility in where they practice.
For more information about which states participate in which compacts, you may check each of above compact websites or search by state at the CCHP Licensure Compacts Page.
The Council of State Governments has also developed a National Center for Interstate Compacts Database that serves as an information clearinghouse related to all interstate compacts in use today. This includes health professions, but is not specific to health professions.
Finally, Provider Bridge is a platform developed to streamline the process for mobilizing health care professionals during the COVID-19 pandemic and for future public health emergencies. It will offer a dedicated customer service hub to help clinicians navigate current state licensure requirements, including those specific to telehealth during states of emergency and provide access to a database of information for verified, betted, volunteer clinicians willing to provide telehealth services during emergencies.
CREDENTIALING AND PRIVILEGING- What does the Joint Commission Require in terms of Privileging when Providing Services Via Telehealth During a Disaster? The applicable requirements that address disaster privileging are found in the Emergency Management (EM) chapter of the Hospital and Critical Access Hospital Accreditation Manuals at EM.02.02.13. NOTE: The disaster privileging option ONLY applies when the organization has implemented their emergency management plan.
Licensed Independent Practitioners (LIP) CURRENTLY credentialed and privileged by the organization, who would now provide the same services via a telehealth link to patients, would not require any additional credentialing or privileging. The medical staff determines which services would be appropriate to be delivered via a telehealth link. There is no requirement that ‘telehealth’ be delineated as a separate privilege.
For volunteer Licensed Independent Practitioners that are NOT currently credentialed and privileged by the organization, disaster privileges may be granted to volunteer LIPs by following the requirements outlined in the Emergency Management chapter of the accreditation manual.
- Are there any CMS Waivers Related to Credentialing and Privileging of Medical Staff? CMS is waiving requirements under 42 CFR §482.22(a)(1)-(4) to allow for physicians whose privileges will expire to continue practicing at the hospital and for new physicians to be able to practice before full medical staff/governing body review and approval to address workforce concerns related to COVID-19. CMS is waiving §482.22(a) (1)-(4) regarding details of the credentialing and privileging process.
Prescribing of Controlled Substances
- Due to the declaration of a public health emergency, the Drug Enforcement Administration (DEA) has made changes to their policies regarding its rules related to prescribing. Review DEA Information on Telemedicine. With that said, please check your State policies, as many States also have laws and regulations governing telehealth and prescribing and these laws and regulations may not have been changes in response to COVID-19.
- Following is a decision tree summarizing the policy changes regarding How to Prescribe Controlled Substances to Patients During the COVID-19 Public Health Emergency
- Historic Background: The Ryan Haight Act of 2008 allowed for certain exemptions to the use of telehealth to provide controlled substances without the telehealth provider having seen the patient in-person first, however these exemptions are narrowly tailored. Two such exemptions are:
1. when a public health emergency (PHE) is declared, and 2. if a provider is registered on a telehealth registry that the Drug Enforcement Administration (DEA) will create.
Such a registry has never been established. In 2018, Congress passed the SUPPORT for Patients and Communities Act as part of an effort to combat the opioid epidemic. The Act directed the DEA to promulgate final regulations for the registry that would allow providers to prescribe controlled substances through telemedicine under certain circumstances. The DEA officially missed its deadline, set at one year from the passing of the Act on October 24, 2019.
-
- A December regulatory posting suggested the DEA plans to publish a proposal, however there was no definitive timeline outlined for the rule’s publication.
- The declaration of a Public Health Emergency (PHE) in March 2020 triggered an allowance in federal law that temporarily allows for the expanded use of telemedicine in prescribing controlled substances for the duration of the PHE. However, that allowance will expire at the end of the PHE.
- In response to the lack of action by the DEA and given the worsening opioid overdose crisis, the Alliance for Connected Care convened more than 80 organizations, who jointly signed a letter urging the DEA to move forward with the telemedicine special registration process required by federal law that will enable SAMHSA waivered clinicians, community mental health centers and addiction treatment facilities to prescribe medication assisted treatment (MAT) drugs to patients with OUD employing telemedicine technology. To read about the issue in more detail and view the letter, see the Alliance for Connected Care’s webpage on the issue.
- In May 2021, Senator Warner sent a letter to Attorney General Merrick Garland regarding the long-delayed regulations and expressed great concern for the delay.
Stay tuned for more updates!
 TELEHEALTH REIMBURSEMENT AND COVID-19
TELEHEALTH REIMBURSEMENT AND COVID-19
About Medicare Reimbursement for Telehealth
- Fee for Service Medicare and Telehealth Reimbursement
-
- Prior to the COVID-19 pandemic, there were a large number of restrictions placed on Fee-for-Service Medicare reimbursement for telehealth services. These restrictions included:
- The originating site (location of the patient). Providers could only get reimbursed for telehealth services if the patients receiving those services were located at specific types of facilities (e.g., hospitals, FQHCs, physician and practitioner offices) AND those facilities were located in specific geographic locations. There were a few exceptions to this rule, such as treatment for Substance Use Disorder, Telestroke and Dialysis for End-State Renal Disease)
- The distant site practitioner (type of provider providing the telehealth service). Only a specific subset of provider types are eligible to serve as distant site providers. This includes Physicians, Nurse Practitioners, Physician Assistants, Nurse Midwives, Clinical Nurse Specialists, Certified Registered Nurse Anesthetists, Clinical Psychologists, Clinical Social Workers and Registered Dietitians or Nutrition Professionals. Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) were specifically excluded from being able to serve as distant site practitioners.
- Types of service. Only a limited set of HCPCS/CPT Codes were eligible for telehealth reimbursement.
- Prior to the COVID-19 pandemic, there were a large number of restrictions placed on Fee-for-Service Medicare reimbursement for telehealth services. These restrictions included:
-
- WHAT'S CHANGED in response to the COVID-19 pandemic? A large number of policy changes that both directly and indirectly impact telehealth have been put into place by CMS as a result of the President's emergency declaration, emergency legislation, waivers and other flexibilities. The Center for Connected Health Policy (The National Telehealth Policy Resource Center) has put together: Billing for Telehealth Encounters: An Introductory Guide on Medicare Fee-For-Service (March 2022). The billing guide seeks to break down permanent post-PHE policies versus temporary PHE policy exceptions, as well as new legislative and administrative requirements relevant to telehealth billing. Many new requirements will only kick in post-PHE. It is important to note that recently passed legislation extends federal temporary waivers under Medicare 151 days after the end of the PHE.
- Telehealth Services During COVID-19 public health emergency: CMS has made available the following resources:
-
-
-
- To see all services approved for billing as a telehealth service, download the List of Telehealth Services for Calendar Year 2022 (includes both temporary and permanent services)
-
-
-
-
-
- The Medicare Learning Network has put together this Telehealth Services Fact Sheet
-
-
-
-
-
- As a companion, also look at the CY2022 Telehealth Update Medicare Physician Fee Schedule
- Finally, CMS has put together this document: COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing. While questions center around a wide variety of topics, there are many related to telehealth.
-
-
-
- Other Virtual Care/Communication (Non-Telehealth) Services During COVID-19 public health emergency: Over the course of the past few years, CMS has been adding several types of Virtual Care/Communication Services that they have deemed to be "Non-Telehealth" Services. Removing these from the definition of telehealth allows these services to be provided without the originating site restrictions that are attached to the traditional definition of telehealth (synchronous video-based) services.
-
-
- Changes to Medicare Virtual Care/Communication (Non-Telehealth) Services as a result of COVID-19:
- The list of clinicians who can provide Virtual Check-Ins and E-Visits has been expanded to include LCSWs, Clinical Psychologists, Physical Therapists, Occupational Therapists and Speech Language Pathologists. Additionally, these visit types can now be provided to not only established patients, but also to new patients.
- Remote physiological monitoring codes may now be provided to not only established patients, but also to new patients.
- FQHCs may now bill for some virtual communication services. See the section in this COVID-19 Telehealth Resources Tookit on Telehealth and FQHCs for more information.
- Changes to Medicare Virtual Care/Communication (Non-Telehealth) Services as a result of COVID-19:
-
-
-
- Billing and Coding for Virtual Care/Communication (Non-Telehealth) Services: Because CMS does not consider these types of service as telehealth services, DO NOT use POS 02 or modifier 95 when billing for these service. CaravanHealth has developed a set of outstanding resources for how and when these billing codes can/should be used:
- At-A-Glance Overview of all Virtual Care and Care Management Services with their corresponding billing codes, examples of their use, brief descriptions and more.)
- Billing and Coding for Virtual Care/Communication (Non-Telehealth) Services: Because CMS does not consider these types of service as telehealth services, DO NOT use POS 02 or modifier 95 when billing for these service. CaravanHealth has developed a set of outstanding resources for how and when these billing codes can/should be used:
-
-
- Other Telehealth-Related Policy Changes During COVID-19
- CMS is allowing physicians to supervise their clinical staff using virtual technologies when appropriate, instead of requiring in-person presence and also allowing hospitals to use other practitioners such as PAs and NPs to the fullest extent possible.
- CMS is loosening "Stark Law" (physician self-referral law) restrictions.
- CMS is allowing telehealth to fulfill many face-to-face visit requirements for clinicians to see their patients in inpatient rehabilitation facilities, hospice and home health.
- CMS is waiving certain conditions of participation requirements, including the requirements regarding telemedicine service agreements.
- Other Telehealth-Related Policy Changes During COVID-19
- Accountable Care Organization (ACO) and Medicare Telehealth Reimbursement
- CMS has developed this Medicare Shared Shavings Program guidance
- CMS has also extended the Next Generation ACO Model to December 2021 (originally set to sunset at the end of 2020). The Next Generation ACO provides an expanded telehealth reimbursement policy compared to Medicare’s pre-COVID-19 telehealth policy, offering participating entities the option to offer telehealth to patients in any geographic area and originating site (including the home) and allowing asynchronous telehealth coverage of dermatology and ophthalmology.
- See a Summary of CMS Innovation Center Models COVID-19 Related Adjustments
- CaravanHealth has developed this Guidance on Collecting Clinical Quality Measures in a Virtual Visit
- CaravanHealth has also developed HCC Capture for Telehealth and Virtual Care Management for ACOs
- FQHCs and RHCs and Medicare Telehealth Reimbursement. In addition to the document above regarding changes authorized by CMS for FQHCs and RHCs, Medicare has also issued this more specific guidance document for FQHCs and RHCs: New and Expanded Flexibilities for RHCs and FQHCs During the COVID-19 Public Health Emergency - Revised January 13, 2022.
-
- If you are an RHC or rural hospital, the National Rural Health Resource Center has put together this webinar on Telehealth Coding and Billing to Maximize Reimbursement. The purpose of the webinar is to provide an overview of coding, billing, and reimbursement updates for telehealth and virtual communication services in CY2021. BKD experts share the status of Medicare public health emergency waivers for telehealth and virtual communication services and discuss pertinent updates for coding, documentation, and billing of telehealth and virtual communication services in the hospital and RHC setting.
-
- If you are an RHC, you may also want to take a look at this CMS MLN Update for Rural Health Clinics.
-
- If you are an FQHC, please visit our section in this COVID-19 Telehealth Resources Tookit on Telehealth and the Federally Qualified Health Center (FQHC) for additional information regarding telehealth related policies such as Scope of Service, FTCA, Medicare Reimbursement, and Telehealth Program Development.
- Medicare Advantage (MA) Plans and Medicare Telehealth Reimbursement
- CMS released final rules for changes to MA plans regarding telehealth in April 2019. The Center for Connected Health Policy has put together this Final Rules for Medicare Advantage Plans and Telehealth Fact Sheet. CMS has also issued this guidance document for Medicare Advantage and Part D Plans.
-
- In response to the pandemic, MA Plans were informed by CMS through this memo that if they wish to expand coverage of telehealth services beyond what has already been approved by CMS, they will exercise its enforcement discretion until it is determined that it is no longer necessary in conjunction with the COVID-19 outbreak.
- Opioid Treatment Programs and Medicare Telehealth Reimbursement
- To address the opioid crisis, Congress passed the “Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities” (SUPPORT) Act that expands Medicare coverage for Opioid Use Disorder (OUD) treatment services. CMS created a bundled payment for the management and counseling for OUD for clinicians in an office setting that is similar to the services under the new OTP benefit for Opioid Treatment Programs and these bundled payment codes became effective on January 1, 2020. Detailed information may be found in the Opioid Treatment Programs (OTPs) Medicare Billing and Payment Fact Sheet. The individual psychotherapy, group therapy, and substance use counseling included in these codes could be furnished using Medicare telehealth services. When using telehealth services for substance use disorder:
- Patients with OUD and SUD can use all originating sites for telehealth services except renal dialysis facilities.
- OUD individual therapy, group therapy, and substance abuse counseling services provided by OTPs must use OTP bundled codes for reimbursement.
- There are no geographic restrictions for telehealth services for OUD, SUD, and co-occurring mental health treatment.
- Patient’s homes can be used as an originating site, but cannot bill a facility fee.
- To address the opioid crisis, Congress passed the “Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities” (SUPPORT) Act that expands Medicare coverage for Opioid Use Disorder (OUD) treatment services. CMS created a bundled payment for the management and counseling for OUD for clinicians in an office setting that is similar to the services under the new OTP benefit for Opioid Treatment Programs and these bundled payment codes became effective on January 1, 2020. Detailed information may be found in the Opioid Treatment Programs (OTPs) Medicare Billing and Payment Fact Sheet. The individual psychotherapy, group therapy, and substance use counseling included in these codes could be furnished using Medicare telehealth services. When using telehealth services for substance use disorder:
-
- In response to the pandemic, CMS is allowing audio-only telephone calls for the therapy and counseling portions of the weekly bundles and the add-on code for additional counseling or therapy for beneficiaries with opioid use disorders without access to interactive audio-video communication technology, provided all other requirements are met.
- Electronic Clinical Quality Measures (eCQMs) and Telehealth.
- CMS has issued this Telehealth Guidance for Electronic Clinical Quality Measures (eCQMs) for Eligible Professional/Eligible Clinician 2021 Quality Reporting. There are 39 telehealth-eligible eCQMs for the 2021 performance period. This guidance applies to the following programs:
- Quality Payment Program: The Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (Advanced APMs)
- APM: Comprehensive Primary Care Plus (CPC+)
- APM: Primary Care First (PCF)
- Medicaid Promoting Interoperability Program for Eligible Professionals
- CMS has issued this Telehealth Guidance for Electronic Clinical Quality Measures (eCQMs) for Eligible Professional/Eligible Clinician 2021 Quality Reporting. There are 39 telehealth-eligible eCQMs for the 2021 performance period. This guidance applies to the following programs:
- I Submitted a Telehealth Claim and It Was Denied. Now What? First make sure that the claim was for an eligible service. To see all services approved for billing as a telehealth service: download the List of Telehealth Services for Calendar Year 2022 (includes both temporary and permanent services). If you are pretty confident that you have been compliant, it is possible that there was a breakdown in communication or misinterpretation of guidance somewhere between CMS and the Medicare Administrative Contractor (MAC) and on down to the individuals who handle the day to day processing of claims. There are multiple MACs and each covers a geographic jurisdiction and handles the processing of medical claims. You will need to contact the MAC for your region to better understand why the claim was denied.
If you have done all of these things and were still denied, please let us know. We also welcome finding out about any other significant challenges related to Medicare reimbursement for telehealth services you are encountering, specifically in relationship to your ability to provide and be reimbursed for patient care as a result of this pandemic. Please be very specific if you contact us (what type of facility/provider is doing the billing, what CPT/E&M codes are being billed, where the patient is getting care, what modifiers are being used and what the specific issue is that is creating the angst). We may be able to get quick attention to some of these issues from CMS if we are hearing the same issues from multiple providers.
About Medicaid Reimbursement for Telehealth
- State Telehealth Laws and Reimbursement Policies: Spring 2021 Executive Summary: A Comprehensive Scan of 50 States and D.C. Findings & Highlights.
- State Telehealth Laws and Reimbursement Policies: At A Glance Spring 2021
- State Telehealth Laws and Reimbursement Policies: Summary Chart Spring 2021
About Private Payer Reimbursement for Telehealth
- Aetna - COVID-19 Service Enhancements
- Aetna - COVID-19 Approved Behavioral Health Telemedicine Services
- AmeriHealth New Jersey - COVID-19 Service Enhancements
- Anthem - COVID-19 Service Enhancements
- Blue Cross and Blue Shield Companies - COVID-19 Service Enhancements
- Blue Cross and Blue Shield of North Carolina - COVID-19 Service Enhancements
- Blue Cross and Blue Shield Federal Employee Program - COVID-19 Service Enhancements
- Capital Blue Cross - COVID-19 Service Enhancements
- CareFirst - COVID-19 Service Enhancements
- CareFirst BlueCross BlueShield - COVID-19 Service Enhancements
- Centene - COVID-19 Service Enhancements
- Cigna - COVID-19 Service Enhancements
- Geisinger Health Plan - COVID-19 Service Enhancements
- Highmark - COVID-19 Service Enhancements
- Horizon Blue Cross Blue Shield of NJ - COVID-19 Service Enhancements
- Humana - COVID-19 Service Enhancements
- Magellan Health - COVID-19 Service Enhancements
- Optima - COVID-19 Service Enhancements
- United Health Care - COVID-19 Telehealth Services
- United Health Care - COVID-19 Physical, Occupational and Speech Therapy Telehealth
- Virginia Premier - COVID-19 Service Enhancements
- State Telehealth Laws and Reimbursement Policies: Spring 2021 Executive Summary: A Comprehensive Scan of 50 States and D.C. Findings & Highlights.
- State Telehealth Laws and Reimbursement Policies: At A Glance Spring 2021
- State Telehealth Laws and Reimbursement Policies: Summary Chart Spring 2021
About Tricare Reimbursement for Telehealth
Specialty Specific Billing and Coding Resources for Clinicians and Practices
- Following are several guidance documents related to billing and coding developed for specific professions/specialty areas as a result of COVID-19:
COVID-19 Claims Reimbursement for Testing and Treatment of the Uninsured
- What is the COVID-19 Claims Reimbursement to Health Care Providers and Facilities for Testing and Treatment of the Uninsured Program? The COVID-19 Claims Reimbursement to Health Care Providers and Facilities for Testing and Treatment of the Uninsured Program provides reimbursements on a rolling basis directly to eligible providers for claims that are attributed to the testing and treatment of COVID-19 for uninsured individuals. The program is authorized via the:
-
- Families First Coronavirus Response Act (P.L. 116-127) and the Paycheck Protection Program and Health Care Enhancement Act (P.L. 116-139), which each appropriated $1 billion to reimburse providers for conducting COVID-19 testing for the uninsured; and the
- CARES Act (P.L. 116-136), which provides $100 billion in relief funds, including to hospitals and other health care providers on the front lines of the COVID-19 response. Within the Provider Relief Fund, a portion of the funding will be used to support healthcare-related expenses attributable to the treatment of uninsured individuals with COVID-19. Funding is provided from the Public Health and Social Services Emergency Fund.
- Who is eligible for funding? Health care providers who have conducted COVID-19 testing of uninsured individuals for COVID-19 or provided treatment to uninsured individuals with a COVID-19 diagnosis on or after February 4, 2020, can request claims reimbursement through the program electronically and will be reimbursed generally at Medicare rates, subject to available funding.
- What services are eligible for reimbursement? Reimbursement will be made for qualifying testing for COVID-19 and treatment services with a primary COVID-19 diagnosis as determined by HRSA (subject to adjustment as may be necessary) , including the following:
- Specimen collection, diagnostic and antibody testing.
- Testing-related visits including in the following settings: office, urgent care or emergency room or via telehealth.
- Treatment, including office visit (including via telehealth), emergency room, inpatient, outpatient/observation, skilled nursing facility, long-term acute care (LTAC), acute inpatient rehab, home health, DME (e.g., oxygen, ventilator), emergency ambulance transportation, non-emergent patient transfers via ambulance, and FDA-approved drugs as they become available for COVID-19 treatment and administered as part of an inpatient stay.
- FDA-approved vaccine, when available.
- For inpatient claims, date of admittance must be on or after February 4, 2020.
View all Frequently Asked Questions about the Program
Provider Relief Fund for Eligible Providers
- $8.5 billion from the American Rescue Plan (ARP) for providers who serve rural Medicaid, Children’s Health Insurance Program (CHIP), or Medicare patients.
- $17 billion for Provider Relief Fund (PRF) Phase 4 payments for a broad range of providers who can document revenue loss and expenses associated with the pandemic.
 TELEHEALTH AND THE FEDERALLY QUALIFIED HEALTH CENTER (FQHC)
TELEHEALTH AND THE FEDERALLY QUALIFIED HEALTH CENTER (FQHC)
Scope of Service and BPHC Policies
- Do health centers need to request a change in scope for a provider to deliver in-scope services via telehealth from their home or another site not on Form 5B, assuming all the criteria for doing so (see question above) are met? (Added: 4/7/2020) Health centers do not need to request a change in scope to deliver in-scope services via telehealth on behalf of the health center from the provider’s home or from another location that is not a Form 5B Service Site. In addition, health centers do not need to have "Home Visits" listed on their Form5C: Other Activities/ Locations in order to provide in-scope services via telehealth.
- May health centers provide in-scope services through telehealth to individuals who are not current health center patients? (Added: 3/19/2020) As a result of the Secretary's declaration relating to the current COVID-19 public health emergency, health center providers may deliver in-scope services via telehealth to individuals who have not previously presented for care at a health center site and who are not current patients of the health center for the duration of this public health emergency. This includes triage services, including initial consultations. Telehealth visits are within the scope of project if:
- The individual receives an in-scope required or additional health service;
- The provider documents the service in a patient medical record consistent with applicable standards of practice; and
- The provider is physically located at a health center service site or at some other location on behalf of the health center (e.g., provider’s home, emergency operations center).
Health centers should focus services provided by telehealth on serving patients and other individuals located inside their service area or with areas adjacent to the covered entity’s service area. HRSA recognizes that patients outside these areas may seek health center screenings and triage by telehealth. Health centers that continue to maintain services for target populations in their service area and provide occasional in-scope services via telehealth to individuals outside these areas would be providing services within the Health Center Program scope of project for all such activities. Please review PAL 2020-01: Telehealth and Health Center Scope of Project (PDF – 520 KB) for more information.
- Can a health center use telehealth to provide services to a patient at a location that is not an in-scope service site? Can this occur if neither the health center provider nor the patient is at an in-scope service site (e.g. both the provider and patient are at their respective homes)? (Updated: 4/7/2020) From a Health Center Program scope of project policy perspective, using telehealth to provide services to a patient at a location that is not an in-scope service site is allowable if:
-
-
- The service being provided via telehealth is within the health center's approved scope of project (recorded on Form 5A);
- The clinician delivering the service is a health center provider working on behalf of the health center; and
- The individual receiving the service is a health center patient.
-
HRSA strongly encourages health centers that provide, or are planning to provide, health services via telehealth to consult with professional organizations, regulatory bodies, and private counsel to help assess, develop, and maintain written telehealth policies that are compliant with Health Center Program requirements; federal, state, and local requirements; and applicable standards of practice. HRSA also encourages health centers to consider the range of issues that would support successful implementation of telehealth. Please review PAL 2020-01: Telehealth and Health Center Scope of Project (PDF – 520 KB) for more information.
- How does telehealth impact my 2020 UDS Clinical Measure Reporting? Please refer to this document for guidance.
Federal Tort Claims Act (FTCA)
- Does FTCA coverage extend to telehealth visits with both established patients and non-health center patients? (Updated: 3/27/2020). When in-scope services are provided through telehealth on behalf of a deemed health center to either established patients or individuals who are not patients of the health center, and all other FTCA Program requirements are met, such services are eligible for liability protections under 42 U.S.C. 233(g)-(n), pursuant to 42 CFR 6.6. Health centers and providers are encouraged to consult with private counsel and/or consider the purchase of private malpractice insurance when undertaking activities that may not be within the health center’s scope of project.
- Will HRSA issue a particularized determination for health centers related to COVID-19 activities, similar to the particularized determination that was issued during the H1N1 emergency? (Added: 3/31/2020). HRSA has issued a particularized determination for health center providers (PDF - 35 KB) that clarifies eligibility for FTCA coverage during the COVID-19 pandemic for the provision of grant-supported health services by individuals who have been deemed as Public Health Service employees through the Health Center FTCA Program and the Health Center VHP FTCA Program. It applies to grant-supported health services to prevent, prepare, or respond to COVID-19 (including but not limited to screening, triage, testing, diagnosis, and treatment) to individuals who are established or non-established patients of the health center, whether in person at the health center, offsite (including at offsite programs or events carried out by the health center), or via telehealth.
- During the declared COVID-19 emergency, do FTCA protections apply to health center providers who provide telehealth services to health center patients located across state lines? (Added: 4/8/2020) Health Center FTCA Program regulations at 42 CFR Part 6 provide that coverage applies to “grant-related activities.” Therefore, a key determinant for FTCA coverage is whether the covered entity is providing services within the health center’s scope of project, under the Health Center Program authorizing statute.
PAL 2020-01: Telehealth and Health Center Scope of Project (PDF - 517 KB) highlights some of the relevant considerations for health centers in providing in-scope services through telehealth. Among other things, all providers must comply with applicable state requirements. If they do not—for example, if a provider uses a state license to provide services in a different state where doing so is unlawful under applicable state law—this may jeopardize eligibility for FTCA liability protection. However, some states may have temporarily amended their requirements for providing health care through telehealth to address the needs of the COVID-19 public health emergency.
Health centers that are uncertain of the applicable legal requirements for the provision of health services through telehealth across state lines should consult their private counsel for advice. HRSA cannot provide general assurance of FTCA coverage in all situations, as such determinations are fact-specific. As stated in the FTCA Health Center Policy Manual (PDF - 407 KB), “[w]hen FTCA matters become the subject of litigation, the Department of Justice and the federal courts assume significant roles in certifying or determining whether or not a given activity falls within the scope of employment for purposes of FTCA coverage.”
- Will a deemed health center’s providers remain covered by liability protections under the FTCA if they are directed to provide continuous or permanent services to non-health center inpatients at a local hospital as part of a community-wide emergency response during the declared COVID-19 public health emergency? (Added: 4/16/2020) Continuous or permanent staffing of a hospital or hospital department to provide inpatient care to all hospital patients is not described by the authorizing statute for the Health Center Program, and FTCA coverage generally is not available for such care.
Health centers have discretion to enter into contractual arrangements with hospitals or may allow their providers to enter into arrangements with hospitals to provide hospital-based inpatient care outside the scope of their Health Center Program grants. However, FTCA coverage and other federal benefits directly associated with the Health Center Program would not apply. Providers providing continuous or permanent inpatient care in hospitals through such arrangements may have medical malpractice liability protection through the hospital or another source, and volunteer providers may be eligible for liability protections under federal and state law (including new legal protections for volunteer providers for COVID-19 emergency response via the CARES Act). Health centers should consult with private counsel for legal advice regarding these matters.
Please note that the Health Center FTCA Program regulations and the March 27, 2020, Determination of Coverage for COVID-19-Related Activities by Health Center Providers (PDF - 35 KB) provide for FTCA protection for deemed health centers in the circumstances described in those issuances. The March 27, 2020, Determination of Coverage indicates that health center providers may provide grant-supported health services “to prevent, prepare, or respond to COVID-19 (including but not limited to screening, triage, testing, diagnosis, and treatment)” to individuals who are not patients of the health center, whether at the health center or off-site, and whether in-person or through telehealth. This determination of coverage extends to local COVID-19 community-wide emergency response activities supported by the health center. The Health Center FTCA Program regulations also provide for liability protections for certain described individual emergency situations.
The Health Center Program provides grant support for the delivery of primary and preventive health care service to medically underserved populations and communities. Services provided through the Health Center Program generally consist of outpatient, ambulatory care services for health center patients. As provided for by statute, regulation, and determination of coverage, services may be provided to individuals who are not patients of the health center in limited circumstances.
Medicare and Medicaid Reimbursement
- What policy changes for FQHCs have been instituted as a result of the pandemic? This video will provide an overview of the CMS policy changes for FQHCs:
This Medicare Learning Network Booklet for Federally Qualified Health Centers provides guidance around Telehealth Services Payment, Virtual Communication Services as well as COVID-19 Flexibilities pertaining to payment. Medicare has also issued this more specific guidance document for FQHCs and RHCs: New and Expanded Flexibilities for RHCs and FQHCs During the COVID-19 Public Health Emergency - Revised January 13, 2022. Additionally, CMS has put together this document: COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing. Questions center around a wide variety of topics, but there is a section specific to FQHCs many of the questions relate to telehealth as well as virtual communication services..
- Can health centers bill Medicare for telehealth services as distant site providers? The Coronavirus Aid, Relief, and Economic Security (CARES) Act revises the definition of a distant site in section 1834(m)(2)(A) of the Social Security Act to include FQHCs or RHCs that furnish a telehealth service to an eligible telehealth individual during the COVID-19 public health emergency period. Rural and site limitations are removed, so that telehealth services furnished during the emergency period can be provided regardless of the geographic location of the Medicare beneficiary, including if the patient is at home. In order to be eligible for reimbursement, providers must use telecommunication systems with both audio and video capabilities for two-way, real-time interactive communication.
Distant site telehealth services can be furnished by any health care practitioner working for the RHC or the FQHC within their scope of practice. Practitioners can furnish distant site telehealth services from any location, including their home, during the time that they are working for the RHC or FQHC, and can furnish any telehealth service, including medical outpatient office visits, behavioral health services, and other visits currently eligible under the Medicare telehealth reimbursement policies. To see all services approved for billing as a telehealth service, download the List of Telehealth Services for Calendar Year 2022 (includes both temporary and permanent services)
- Is there current guidance on the reimbursement methodology for distant site telehealth visits under Medicare? See the Medicare guidance document New and Expanded Flexibilities for RHCs and FQHCs During the COVID-19 Public Health Emergency - Revised January 13, 2022.
- Will I be required to get patient consent for telehealth and virtual communication services? Consent is not required for telehealth services. However, beneficiary consent is required for care management and virtual communication services. During the public health emergency (PHE), beneficiary consent may be obtained at the same time the services are initially furnished. For FQHCs, this means that beneficiary consent can be obtained by someone working under general supervision of the FQHC practitioner, and direct supervision is not required to obtain consent. In general, beneficiary consent to receive these services may be obtained by auxiliary personnel under general supervision of the billing practitioner; and the person obtaining consent can be an employee, independent contractor, or leased employee of the billing practitioner. For FQHCs, beneficiary consent to receive these services may be obtained by auxiliary personnel under general supervision of the FQHC practitioner; and the person obtaining consent can be an employee, independent contractor, or leased employee of the FQHC practitioner (see: https://www.cms.gov/files/document/covid-final-ifc.pdf).
- Are there telehealth services where cost sharing has been waived as a result of the pandemic? There are several CPT and HCPCS codes that describe preventive services and should be billed as G2025. When provided by telehealth, cost sharing requirements are waived for these services. .
- What policies have not changed for FQHCs as a result of the pandemic?
- Remote Patient Monitoring (RPM)/Remote Physiologic Monitoring (99453, 99454): CMS clarified toward the end of 2019 that RPM services are not separately billable under Medicare for FQHCs. Since the FQHC Prospective Payment System (PPS) rate includes all services and supplies furnished ‘incident to’ the visit,” CMS feels that RPM costs are already included in the FQHC PPS payment.
-
- eConsult or Interprofessional Consultations (99446-99449, 99451, 99452): CMS guidance says that FQHCs cannot bill for eConsults under Medicare.
- Following is CMS guidance on the New and Expanded Flexibilities for RHCs and FQHCs During the COVID-19 Public Health Emergency - Revised January 13, 2022.
- To see all services approved for billing as a telehealth service: download the List of Telehealth Services for Calendar Year 2022 (includes both temporary and permanent services)
- To receive payment for telephone (audio-only) evaluation and management services (CPT codes 99441, 99442, and 99443) , FQHCs should use HCPCS code G2025. To bill for these services, at least 5 minutes of telephone E/M service by a physician or other qualified health care professional who may report E/M services must be provided to an established patient, parent, or guardian. These services cannot be billed if they originate from a related E/M service provided within the previous 7 days or lead to an E/M service or procedure within the next 24 hours or soonest available appointment.
- To receive payment for online digital evaluation and management services (non-face-to-face, patient-initiated, digital communications using a secure patient portal):
- CPT code 99421 (5-10 minutes over a 7 day period)
- CPT code 99422 (11-20 minutes over a 7 day period)
- CPT code 99423 (21 minutes or more over a 7 day period)
and virtual communication services (HCPCS codes G2012 and G2010), FQHCs must submit an FQHC claim with HCPCS code G0071 (Virtual Communication Services) either alone or with other payable services. For claims submitted with HCPCS code G0071 on or after March 1, 2020, and for the duration of the COVID-19 PHE, payment for HCPCS code G0071 is set at the average of the national non-facility PFS payment rates for these 5 codes. Claims submitted with G0071 on or after March 1 and for the duration of the PHE will be paid at the new rate of $24.76, instead of the CY 2020 rate of $13.53. MACs will automatically reprocess any claims with G0071 for services furnished on or after March 1 that were paid before the claims processing system was updated.
- CaravanHealth put together these two documents that you may find useful:
- Costs for furnishing distant site telehealth services will not be used to determine the FQHC PPS rates but must be reported on the appropriate cost report form. FQHCs must report both originating and distant site telehealth costs on Form CMS-224-14, the Federally Qualified Health Center Cost Report, on line 66 of the Worksheet A, in the section titled “Other FQHC Services”. Since telehealth distant site services are not paid under tthe FQHC PPS, the Medicare Advantage wrap-around payment does not apply to these services. Wrap-around payment for distant site telehealth services will be adjusted by the MA plans.
- NACHC has prepared this Resource Guide on Telehealth Coverage in Medicaid that outlines Medicaid coverage at Health Centers during the pandemic and provides tools for policy changes and recommendations moving forward.
Telehealth Program Development and the Future of Telehealth for FQHCs
- The National Consortium of Telehealth Resource Centers (NCTRC) has a Collection of FQHC Telehealth Resources that is a curation of resources developed by all of the TRCs and designed specifically for FQHCs! This is a great place to start. A few highlights from this collection include:
- Recorded content from the three session FQHC Webinar Series:
- In addition, the Health Center Resource Clearinghouse also has a Collection of COVID-19 Resources for Telehealth.
- Beyond the abundance of materials found in these clearinghouses, here are a few other FQHC specific resources::
-
- We offered a 2-Hour Session on Telehealth in Community Health Centers during our 2019 Telehealth Summit. In this screencast, you will take a closer look at successful established telehealth program models found in FQHCs.
-
- The Center for Care Innovations has put together Telehealth and Telephone Visits in the Time of COVID-19: FQHC Workflows and Guides.
-
- The National School-Based Health Alliance has developed this School-Based Telehealth Playbook for FQHCs as part of a Youth Safety Net Project.
-
- The Health Information Technology, Evaluation, and Quality Center (HITEQ) has put together several useful toolkits and resources, including:
- Getting a New Workflow and Process Started During COVID-19 Pandemic as a quick start guide for health centers (please note that Remote Patient Monitoring billing codes are included in this document - CMS has clarified that RPM services are not separately billable under Medicare for FQHCs. Since the FQHC Prospective Payment System (PPS) rate include all services and supplies furnished ‘incident to’ the visit,” RPM is theoretically already included in the FQHC PPS payment).
- Using Telehealth to Expand PrEP Access in Health Centers. This brief highlights how health centers are using telehealth resources and innovations for HIV Pre-Exposure Prophylaxis (PrEP)
- Electronic Patient Engagement (EPE) Tool Inventory. In the spring of 2020, HITEQ and several PCA and HCCN colleagues developed a survey to gather detailed information on health center experiences with a variety of EPE tools and included questions about product functions, strengths & weaknesses, cost, integration with EHRs, ease of implementation, and quality of vendor support. The results of that survey, as well as interviews and demonstrations are captured in this EPE Tool Inventory.
- The Health Information Technology, Evaluation, and Quality Center (HITEQ) has put together several useful toolkits and resources, including:
-
- The Weitzman Institute provides a series of Project ECHO Clinics on a wide variety of topics geared specifically for FQHCs, many of which include telehealth integrated care models.
-
- The following vendors are offering access to eConsult services for FQHCs during the pandemic. Please note that MATRC is not in a position to either endorse or recommend any of the vendors on this list. We strongly encourage you to do your due diligence when making a vendor selection:
- Free access to Safety Net Connect eConsult Telehealth Portal for primary care physicians
- Free access to ConferMED Coronavirus eConsults for Safety Net Practices
- Free access to The MAVEN Project for eConsults for community health clinics who serve the underserved (The MAVEN Project is available without charge even beyond the pandemic)
- The following vendors are offering access to eConsult services for FQHCs during the pandemic. Please note that MATRC is not in a position to either endorse or recommend any of the vendors on this list. We strongly encourage you to do your due diligence when making a vendor selection:
- How the Rapid Shift to Telehealth Leaves Many Community Health Centers Behind During the COVID-19 Pandemic (Health Affairs)
- Barriers & Challenges to FQHC Use of Telehealth for Substance Use Disorder: A Examination of Policies Affecting FQHCs Pre- and During COVID-19 Emergency (Center for Connected Health Policy)
- Telehealth Practice Among Health Centers During the COVID-19 Pandemic - United States, July 11 - 17, 2020 (CDC)
- Telemedicine Services During COVID-19: Considerations for Medically Underserved Populations (The Journal of Rural Health)
- Community Health Centers COVID-19 Digital Inequities Impacting Access (CaliforniaHealth)
 WHAT HAPPENS WHEN THE PANDEMIC IS OVER?
WHAT HAPPENS WHEN THE PANDEMIC IS OVER?
Transitioning from Temporary to Permanent Policies
- The US Health and Human Services has officially renewed the public health emergency (PHE) on multiple occasions, a status that allows many of the waivers and expansions for telehealth that have occurred since the COVID-19 pandemic began in March 2020 to remain active. Each renewal extends the PHE an additional 90 days. The latest renewal, which occurred on April 13, 2022 extends the PHE through July 11, 2022. Key regulatory flexibilities linked to the PHE include the 1135 Waivers, the CMS Interim Final Rule, a number of initiatives under the Families First Coronavirus Response Act and CARES Act legislation, several State Medicaid and CHIP Program flexibilities, HIPAA Enforcement Discretion, Fraud and Abuse Enforcement Discretion and Flexibility Regarding Controlled Substances. Click here for a recent analysis of what policies are linked to the PHE and what are not.
- While the above discusses the status of the federal PHE, many states have already ended their PHE declarations. The Center for Telehealth and eHealth Law (CTeL) has created a 50 State Survey of the status of the PHE for each state. for its members. This is a view of what that survey looks like for July 12. To get ongoing updates, you would need to join CTeL as a member.
- Here is a look at what temporary policy changes might remain post-COVID-19 and what could be issues that policymakers my think merit future action:
- There were some significant changes in telehealth reimbursement as a result of the pandemic and it is likely that the reimbursement, coding and billing policies will eventually revert back to their pre-pandemic guidance. This video provides a really good overview about how telehealth is reimbursed in the U.S., the impact of the public health emergency and some thoughts on how to think about it after the public health emergency:
- This Billing for Telehealth Encounters: An Introductory Guide on Fee-For-Service is a great tool for helping you navigate reimbursement and understand what changes are temporary vs. permanent. Although much of its focus is on fee-for-service Medicare, it also provides information about Medicaid and private payor coverage. In addition, this document also discusses how to bill and code for several types of services that CMS does not consider "telehealth". These include: Remote Communication Technology, Virtual Check-In, Remote Evaluation of Pre-Recorded Patient Information and Interprofessional Internet Consultation.
- To get an even better understanding of Fee for Service Medicare policies, review this document Fee for Service Medicare Telehealth Services and Click Here to see a compilation of questions to CMS related to telehealth reimbursement for FFS Medicare and their responses.
- The Center for Connected Health Policy has been capturing State Medicaid policy related changes (both temporary and permanent) through a webinar series. The Winter and Spring Series webinars were recorded and can be viewed by clicking on the links below.
- Winter 1: Waivers and State Plan Amendments to Address COVID-19
- Winter 2: Provider Engagement & Education During the Public Health Emergency
- Winter 3: Patient Engagement & Education During the Public Health Emergency
- Winter 4: What's Next? A Roadmap for Medicaid Telehealth Policy Beyond the Pandemic
For a written summary of the Winter Series: Telehealth & Medicaid: A Policy Webinar Series - Winter Webinar Series Report
For a written summary of the Spring Series: Medicaid & Telehealth: Summary and Findings from Spring Webinar Series
A Quick Overview of The Flurry of Activities Already Underway to Make Temporary Changes Permanent:- This video provides you with an overview of how telehealth policy is structured in the U.S:
- Here are a number of reports regarding policies and policy recommendations as a result of our experience with COVID-19:
-
- Barriers & Challenges to FQHC Use of Telehealth for Substance Use Disorder: A Examination of Policies Affecting FQHCs Pre- and During COVID-19 Emergency (Center for Connected Health Policy)
- Navigating COVID-19: Health Policy Solutions - Telehealth (Missouri Foundation for Health)
- Removing Regulatory Barriers to Telehealth Before and After COVID-19 (Brookings)
- Telemedicine Services During COVID-19: Considerations for Medically Underserved Populations (The Journal of Rural Health)
- Telehealth & COVID-19 Policy Considerations to Improve Access to Care (UCLA Latino Policy & Politics Initiative/UCLA Health Center for the Study of Latino Health and Culture)
- How the Rapid Shift to Telehealth Leaves Many Community Health Centers Behind During the COVID-19 Pandemic (Health Affairs)
- Taskforce on Telehealth Policy: Findings and Recommendations (NCQA)
- Assessing Legal Responses to COVID-19 (Public Health Law Watch)
- Building a Modern Health Care System: Recommendations from the COVID-19 Federal Policy Work Group (eHealth Initiative)
- Community Health Centers COVID-19 Digital Inequities Impacting Access (CaliforniaHealth)
- Report to Congress: Medicare Payment Policy (MEDPAC)
- The Future of State Telehealth Policy (National Governors Association)
- Medicare and Medicaid: COVID-19 Program Flexibilities and Considerations for Their Continuation (U.S. Government Accountability Office)
- Key Findings from RAND Health Care Research on Telehealth Policy (RAND Corporation)
- Cost Benefit Analysis of Telehealth: March 2020 - September 2020 (CTeL)
- Following are some some of the efforts toward policy changes already under way:
- On Wednesday June 17, the U.S. Senate Committee on Health, Education Labor & Pensions held a hearing on Telehealth: Lessons from the COVID-19 Pandemic. Our own Karen S. Rheuban joined Joseph C. Kvedar, Sanjeev Arora and Andrea Willis to share testimony, contributing to the discussion about what temporary telehealth changes should be made permanent in federal and state policies. Watch Here!
-
- On June 29th, 340 organizations signed a letter urging Congressional leaders to make telehealth flexibilities created during COVID-19 pandemic permanent. Read the Letter Here!
-
- The Taskforce on Telehealth Policy had invited public input as it develops policy recommendations for advancing quality and patient experience while establishing a stable, long-term environment that fosters the growth and integration of remote services within the healthcare system. Learn more here.
-
- The American Hospital Association has written an open letter addressed to President Trump regarding the need to do to enable more for hospitals and health systems to provide virtual care.
-
- The Medicare Payment Advisory Commission (MEDPAC) presented policy options for expanding telehealth in Medicare. See the presentation here.
-
- In mid-November, the US Department of Veterans Affairs released an interim final rule allowing VA health care professionals to practice across state lines beyond the COVID-19 public health emergency as long as it is in accordance with the scope and requirements of their VA employment, regardless of state licensing requirements. Read the full interim final rule here.
-
- CMS finalized its CY2021 Physician Fee Schedule and issued this fact sheet The 2021 PFS makes permanent a number of codes that are currently on the Medicare telehealth list as a result of the COVID-19 public health emergency (PHE) and adds others provisionally through the end of the year in which the PHE ends. CMS also addresses a number of other issues, such as frequency limits for nursing facility visits furnished via telehealth. Clarification is given around issues such as the ability of physical, occupational and speech language pathologists to furnish brief online assessment and management services and certain requirements related to remote physiologic monitoring. CMS also specifies that the telehealth restrictions do not apply when a beneficiary and practitioner are in the same location even if conducted via audio/video technology. In the absence of the COVID-19 PHE declaration, CMS will not continue to recognize audio-only codes that were added in 2020 in response to the COVID-19 PHE. However, based on comments received, they are establishing a new HCPCS G-code describing 11-20 minutes of medical discussion to determine the necessity of an in-person visit.
- The Center for Connected Health Policy has also developed this Fact Sheet specific to the telehealth related provisions.
- CMS finalized its CY2021 Physician Fee Schedule and issued this fact sheet The 2021 PFS makes permanent a number of codes that are currently on the Medicare telehealth list as a result of the COVID-19 public health emergency (PHE) and adds others provisionally through the end of the year in which the PHE ends. CMS also addresses a number of other issues, such as frequency limits for nursing facility visits furnished via telehealth. Clarification is given around issues such as the ability of physical, occupational and speech language pathologists to furnish brief online assessment and management services and certain requirements related to remote physiologic monitoring. CMS also specifies that the telehealth restrictions do not apply when a beneficiary and practitioner are in the same location even if conducted via audio/video technology. In the absence of the COVID-19 PHE declaration, CMS will not continue to recognize audio-only codes that were added in 2020 in response to the COVID-19 PHE. However, based on comments received, they are establishing a new HCPCS G-code describing 11-20 minutes of medical discussion to determine the necessity of an in-person visit.
-
- US Rep. Ann Wagner (R-MO) introduced HR 7992 (Telehealth Act) that combines nine telehealth bills into one piece of legislation. The legislation would provide various expansions in Medicare reimbursement for telehealth, including coverage for telemental health services without geographic and site restrictions, allowing FQHCs and RHCs to be distant site providers and more. The nine federal bills include:
- HR 7338: The Advancing Telehealth Beyond COVID-19 Act
- HR 5473: The EASE Behavioral Health Services Act
- S 4039: The Telemedicine Everywhere Lifting Everyone’s Healthcare Experience and Long-Term Health (TELEHEALTH) HSA Act
- HR 3228: The VA Mission Telehealth Clarification Act
- HR 4900: The Telehealth Across State Lines Act
- S 4103: The Telehealth Response for E-prescribing Addiction Therapy Services (TREATS) Act
- HR 7233: The KEEP Telehealth Options Act
- S 3988: The Enhancing Preparedness Through Telehealth Act
- HR 7187: The HEALTH Act
- US Rep. Ann Wagner (R-MO) introduced HR 7992 (Telehealth Act) that combines nine telehealth bills into one piece of legislation. The legislation would provide various expansions in Medicare reimbursement for telehealth, including coverage for telemental health services without geographic and site restrictions, allowing FQHCs and RHCs to be distant site providers and more. The nine federal bills include:
-
- Senator Schatz (S 1512) has introduced the Connect Act for Health - 2021 - this video provides an overview of the key provisions (of which there are many):
-
- CMS has proposed its CY2022 Physician Fee Schedule and issued this fact sheet CMS is soliciting public comments before the policies will be finalized later this year. Public comments are due no later than 5 PM on September 13, 2021. The Center for Connected Health Policy has developed this Fact Sheet specific to the telehealth related provisions.
- If you want a snapshot of telehealth policies for all States, take a look at the following documents:
- For a deeper dive on all State Telehealth reimbursement and reimbursement related policies, visit: https://www.cchpca.org/all-telehealth-policies/
- You may be interested in reading this paper on State Medicaid Medical Directors Network:: Perspectives on Telehealth Modernization
Telehealth Quality and Performance Improvement
- Many federal and state policies were loosened in response to this public health emergency. This has enabled some "sloppy" telehealth care. Start thinking now about changes you will need to make to fix "sloppy" and to ensure you have the right infrastructure and tools in place to meet legal, regulatory and clinical standards of care for your patients/clients. In addition to all of the Best Practices found in this toolkit, here are a few toolks that can help you think about the bigger picture:
- The American Medical Association has put together a really nice Telehealth Implementation Playbook that would be useful once you have the ability to step back from the immediate need to get up and running and to think more strategically for longer term planning.
- The Medical University of South Carolina (MUSC) has put together this Telehealth Service Implementation Model (TSIM): A Framework for Telehealth Service Development, Implementation and Sustainability.
- The California TRC has developed this comprehensive Telehealth Program Developer Kit: A Roadmap for Successful Telehealth Program Development: as well as this Compendium of Best Practices in Telehealth Services.
- The American Academy of Family Physicians has developed A Toolkit for Building and Growing a Sustainable Telehealth Program in Your Practice.
- For those working with rural communities, the Rural Health Information Hub has developed a Rural Telehealth Toolkit
- Don't expect "business as usual". Prepare for a tsunami of patients who have delayed care and will need it. Prepare also for patients who will continue to delay care because they are fearful of exposure by coming into your office or a health care facility. Start thinking NOW about how to use the telehealth tools you have started putting into place to address this oncoming wave. Start thinking now also about quality of care. Here are a few resources to serve as food for thought:
- We have now let the genie out of the bottle and hundreds of thousands of providers and patients will have experienced telehealth for the first time. Some will recognize its value and want to continue. What data should you be collecting now so you can both demonstrate telehealth quality, assess performance improvement and be prepared to make a case for policy changes if/when needed?
- Here is an attempt at a first draft of a COVID-19 Measure Framework developed by SPROUT. It is still a work in progress, but should provide some food for thought.
- CaravanHealth has developed this Guidance on Collecting Clinical Quality Measures in a Virtual Visit
- CMS has issued this Telehealth Guidance for Electronic Clinical Quality Measures (eCQMs) for Eligible Professional/Eligible Clinician 2021 Quality Reporting. There are 39 telehealth-eligible eCQMs for the 2021 performance period. This guidance applies to the following programs:
- Quality Payment Program: The Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (Advanced APMs)
- APM: Comprehensive Primary Care Plus (CPC+)
- APM: Primary Care First (PCF)
- Medicaid Promoting Interoperability Program for Eligible Professionals
- For those wanting to assess implementation, workflows, etc...as these are being together, the Consolidated Framework for Implementation Research is a great place to start.
- We have some preliminary data reports coming out regarding trends and impact on telehealth from COVID-19. Here are several recent ones:
- As the Country Reopens Safety Concerns Rise (Sage Growth/Blackbook Research) does a good job capturing where we are right now
- The Impact of COVID-19 Pandemic on Outpatient Visits: Changing Patterns of Care in the Newest COVID-19 Hot Spots (Commonwealth Fund)
- The Impact of the COVID-19 Pandemic on Outpatient Care: Visits Return to Pre-pandemic Levels, but Not for All Providers and Patients (Commonwealth Fund)
- Medicare Beneficiary Use of Telehealth Visits: Early Data from the Start of the COVID-19 Pandemic (ASPE)
- Monthly Telehealth Regional Tracker (FAIR Health)
- Special Report: The Rapid Transition to Telemedicine Insights and Early Trends (Press Ganey)
- Telehealth Use Among Older Adults Before and During COVID-19 (National Poll on Healthy Aging - University of Michigan)
- Services Delivered via Telehealth Among Medicaid & CHIP Beneficiaries During COVID-19: Preliminary Medicaid & CHIP Data Snapshot for Services through June 30, 2020 (CMS)
- Trends in the Use of Telehealth During the Emergence of the COVID-19 Pandemic - United States, January - March 2020 (CDC)
- COVID-19 Telehealth Impact Study (The COVID-19 Healthcare Coalition Telehealth Impact Study Work Group)
- The Future of Telehealth in School-Based Health Centers: Lessons from COVID-19 (Journal of Pediatric Health Care)
- In-Person and Telehealth Ambulatory Contacts and Costs in a Large US Insured Cohort Before and During the COVID-19 Pandemic (JAMA Network)
- Medicare and Telehealth: Coverage and Use During the COVID-19 Pandemic and Options for the Future (Kaiser Family Foundation)
- Patient Characteristics Associated with the Successful Transition to Virtual Care: Lessons Learned from the First Million Patients ( Mass General Hospital)
About Medicare Reimbursement for Telehealth
- Fee for Service Medicare and Telehealth Reimbursement
-
- Prior to the COVID-19 pandemic, there were a large number of restrictions placed on Fee-for-Service Medicare reimbursement for telehealth services. These restrictions included:
- The originating site (location of the patient). Providers could only get reimbursed for telehealth services if the patients receiving those services were located at specific types of facilities (e.g., hospitals, FQHCs, physician and practitioner offices) AND those facilities were located in specific geographic locations. There were a few exceptions to this rule, such as treatment for Substance Use Disorder, Telestroke and Dialysis for End-State Renal Disease)
- The distant site practitioner (type of provider providing the telehealth service). Only a specific subset of provider types are eligible to serve as distant site providers. This includes Physicians, Nurse Practitioners, Physician Assistants, Nurse Midwives, Clinical Nurse Specialists, Certified Registered Nurse Anesthetists, Clinical Psychologists, Clinical Social Workers and Registered Dietitians or Nutrition Professionals. Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) were specifically excluded from being able to serve as distant site practitioners.
- Types of service. Only a limited set of HCPCS/CPT Codes were eligible for telehealth reimbursement.
- Prior to the COVID-19 pandemic, there were a large number of restrictions placed on Fee-for-Service Medicare reimbursement for telehealth services. These restrictions included:
-
- WHAT'S CHANGED in response to the COVID-19 pandemic? A large number of policy changes that both directly and indirectly impact telehealth have been put into place by CMS as a result of the President's emergency declaration, emergency legislation, waivers and other flexibilities. The Center for Connected Health Policy (The National Telehealth Policy Resource Center) has put together: Billing for Telehealth Encounters: An Introductory Guide on Medicare Fee-For-Service (March 2022). The billing guide seeks to break down permanent post-PHE policies versus temporary PHE policy exceptions, as well as new legislative and administrative requirements relevant to telehealth billing. Many new requirements will only kick in post-PHE. It is important to note that recently passed legislation extends federal temporary waivers under Medicare 151 days after the end of the PHE.
- Telehealth Services During COVID-19 public health emergency: CMS has made available the following resources:
-
-
-
- To see all services approved for billing as a telehealth service, download the List of Telehealth Services for Calendar Year 2022 (includes both temporary and permanent services)
-
-
-
-
-
- The Medicare Learning Network has put together this Telehealth Services Fact Sheet
-
-
-
-
-
- As a companion, also look at the CY2022 Telehealth Update Medicare Physician Fee Schedule
- Finally, CMS has put together this document: COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing. While questions center around a wide variety of topics, there are many related to telehealth.
-
-
-
- Other Virtual Care/Communication (Non-Telehealth) Services During COVID-19 public health emergency: Over the course of the past few years, CMS has been adding several types of Virtual Care/Communication Services that they have deemed to be "Non-Telehealth" Services. Removing these from the definition of telehealth allows these services to be provided without the originating site restrictions that are attached to the traditional definition of telehealth (synchronous video-based) services.
-
-
- Changes to Medicare Virtual Care/Communication (Non-Telehealth) Services as a result of COVID-19:
- The list of clinicians who can provide Virtual Check-Ins and E-Visits has been expanded to include LCSWs, Clinical Psychologists, Physical Therapists, Occupational Therapists and Speech Language Pathologists. Additionally, these visit types can now be provided to not only established patients, but also to new patients.
- Remote physiological monitoring codes may now be provided to not only established patients, but also to new patients.
- FQHCs may now bill for some virtual communication services. See the section in this COVID-19 Telehealth Resources Tookit on Telehealth and FQHCs for more information.
- Changes to Medicare Virtual Care/Communication (Non-Telehealth) Services as a result of COVID-19:
-
-
-
- Billing and Coding for Virtual Care/Communication (Non-Telehealth) Services: Because CMS does not consider these types of service as telehealth services, DO NOT use POS 02 or modifier 95 when billing for these service. CaravanHealth has developed a set of outstanding resources for how and when these billing codes can/should be used:
- At-A-Glance Overview of all Virtual Care and Care Management Services with their corresponding billing codes, examples of their use, brief descriptions and more.)
- Billing and Coding for Virtual Care/Communication (Non-Telehealth) Services: Because CMS does not consider these types of service as telehealth services, DO NOT use POS 02 or modifier 95 when billing for these service. CaravanHealth has developed a set of outstanding resources for how and when these billing codes can/should be used:
-
-
- Other Telehealth-Related Policy Changes During COVID-19
- CMS is allowing physicians to supervise their clinical staff using virtual technologies when appropriate, instead of requiring in-person presence and also allowing hospitals to use other practitioners such as PAs and NPs to the fullest extent possible.
- CMS is loosening "Stark Law" (physician self-referral law) restrictions.
- CMS is allowing telehealth to fulfill many face-to-face visit requirements for clinicians to see their patients in inpatient rehabilitation facilities, hospice and home health.
- CMS is waiving certain conditions of participation requirements, including the requirements regarding telemedicine service agreements.
- Other Telehealth-Related Policy Changes During COVID-19
- Accountable Care Organization (ACO) and Medicare Telehealth Reimbursement
- CMS has developed this Medicare Shared Shavings Program guidance
- CMS has also extended the Next Generation ACO Model to December 2021 (originally set to sunset at the end of 2020). The Next Generation ACO provides an expanded telehealth reimbursement policy compared to Medicare’s pre-COVID-19 telehealth policy, offering participating entities the option to offer telehealth to patients in any geographic area and originating site (including the home) and allowing asynchronous telehealth coverage of dermatology and ophthalmology.
- See a Summary of CMS Innovation Center Models COVID-19 Related Adjustments
- CaravanHealth has developed this Guidance on Collecting Clinical Quality Measures in a Virtual Visit
- CaravanHealth has also developed HCC Capture for Telehealth and Virtual Care Management for ACOs
- FQHCs and RHCs and Medicare Telehealth Reimbursement. In addition to the document above regarding changes authorized by CMS for FQHCs and RHCs, Medicare has also issued this more specific guidance document for FQHCs and RHCs: New and Expanded Flexibilities for RHCs and FQHCs During the COVID-19 Public Health Emergency - Revised January 13, 2022.
-
- If you are an RHC or rural hospital, the National Rural Health Resource Center has put together this webinar on Telehealth Coding and Billing to Maximize Reimbursement. The purpose of the webinar is to provide an overview of coding, billing, and reimbursement updates for telehealth and virtual communication services in CY2021. BKD experts share the status of Medicare public health emergency waivers for telehealth and virtual communication services and discuss pertinent updates for coding, documentation, and billing of telehealth and virtual communication services in the hospital and RHC setting.
-
- If you are an RHC, you may also want to take a look at this CMS MLN Update for Rural Health Clinics.
-
- If you are an FQHC, please visit our section in this COVID-19 Telehealth Resources Tookit on Telehealth and the Federally Qualified Health Center (FQHC) for additional information regarding telehealth related policies such as Scope of Service, FTCA, Medicare Reimbursement, and Telehealth Program Development.
- Medicare Advantage (MA) Plans and Medicare Telehealth Reimbursement
- CMS released final rules for changes to MA plans regarding telehealth in April 2019. The Center for Connected Health Policy has put together this Final Rules for Medicare Advantage Plans and Telehealth Fact Sheet. CMS has also issued this guidance document for Medicare Advantage and Part D Plans.
-
- In response to the pandemic, MA Plans were informed by CMS through this memo that if they wish to expand coverage of telehealth services beyond what has already been approved by CMS, they will exercise its enforcement discretion until it is determined that it is no longer necessary in conjunction with the COVID-19 outbreak.
- Opioid Treatment Programs and Medicare Telehealth Reimbursement
- To address the opioid crisis, Congress passed the “Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities” (SUPPORT) Act that expands Medicare coverage for Opioid Use Disorder (OUD) treatment services. CMS created a bundled payment for the management and counseling for OUD for clinicians in an office setting that is similar to the services under the new OTP benefit for Opioid Treatment Programs and these bundled payment codes became effective on January 1, 2020. Detailed information may be found in the Opioid Treatment Programs (OTPs) Medicare Billing and Payment Fact Sheet. The individual psychotherapy, group therapy, and substance use counseling included in these codes could be furnished using Medicare telehealth services. When using telehealth services for substance use disorder:
- Patients with OUD and SUD can use all originating sites for telehealth services except renal dialysis facilities.
- OUD individual therapy, group therapy, and substance abuse counseling services provided by OTPs must use OTP bundled codes for reimbursement.
- There are no geographic restrictions for telehealth services for OUD, SUD, and co-occurring mental health treatment.
- Patient’s homes can be used as an originating site, but cannot bill a facility fee.
- To address the opioid crisis, Congress passed the “Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities” (SUPPORT) Act that expands Medicare coverage for Opioid Use Disorder (OUD) treatment services. CMS created a bundled payment for the management and counseling for OUD for clinicians in an office setting that is similar to the services under the new OTP benefit for Opioid Treatment Programs and these bundled payment codes became effective on January 1, 2020. Detailed information may be found in the Opioid Treatment Programs (OTPs) Medicare Billing and Payment Fact Sheet. The individual psychotherapy, group therapy, and substance use counseling included in these codes could be furnished using Medicare telehealth services. When using telehealth services for substance use disorder:
-
- In response to the pandemic, CMS is allowing audio-only telephone calls for the therapy and counseling portions of the weekly bundles and the add-on code for additional counseling or therapy for beneficiaries with opioid use disorders without access to interactive audio-video communication technology, provided all other requirements are met.
- Electronic Clinical Quality Measures (eCQMs) and Telehealth.
- CMS has issued this Telehealth Guidance for Electronic Clinical Quality Measures (eCQMs) for Eligible Professional/Eligible Clinician 2021 Quality Reporting. There are 39 telehealth-eligible eCQMs for the 2021 performance period. This guidance applies to the following programs:
- Quality Payment Program: The Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (Advanced APMs)
- APM: Comprehensive Primary Care Plus (CPC+)
- APM: Primary Care First (PCF)
- Medicaid Promoting Interoperability Program for Eligible Professionals
- CMS has issued this Telehealth Guidance for Electronic Clinical Quality Measures (eCQMs) for Eligible Professional/Eligible Clinician 2021 Quality Reporting. There are 39 telehealth-eligible eCQMs for the 2021 performance period. This guidance applies to the following programs:
- I Submitted a Telehealth Claim and It Was Denied. Now What? First make sure that the claim was for an eligible service. To see all services approved for billing as a telehealth service: download the List of Telehealth Services for Calendar Year 2022 (includes both temporary and permanent services). If you are pretty confident that you have been compliant, it is possible that there was a breakdown in communication or misinterpretation of guidance somewhere between CMS and the Medicare Administrative Contractor (MAC) and on down to the individuals who handle the day to day processing of claims. There are multiple MACs and each covers a geographic jurisdiction and handles the processing of medical claims. You will need to contact the MAC for your region to better understand why the claim was denied.
If you have done all of these things and were still denied, please let us know. We also welcome finding out about any other significant challenges related to Medicare reimbursement for telehealth services you are encountering, specifically in relationship to your ability to provide and be reimbursed for patient care as a result of this pandemic. Please be very specific if you contact us (what type of facility/provider is doing the billing, what CPT/E&M codes are being billed, where the patient is getting care, what modifiers are being used and what the specific issue is that is creating the angst). We may be able to get quick attention to some of these issues from CMS if we are hearing the same issues from multiple providers.
About Medicaid Reimbursement for Telehealth
- State Telehealth Laws and Reimbursement Policies: Spring 2021 Executive Summary: A Comprehensive Scan of 50 States and D.C. Findings & Highlights.
- State Telehealth Laws and Reimbursement Policies: At A Glance Spring 2021
- State Telehealth Laws and Reimbursement Policies: Summary Chart Spring 2021
About Private Payer Reimbursement for Telehealth
- Aetna - COVID-19 Service Enhancements
- Aetna - COVID-19 Approved Behavioral Health Telemedicine Services
- AmeriHealth New Jersey - COVID-19 Service Enhancements
- Anthem - COVID-19 Service Enhancements
- Blue Cross and Blue Shield Companies - COVID-19 Service Enhancements
- Blue Cross and Blue Shield of North Carolina - COVID-19 Service Enhancements
- Blue Cross and Blue Shield Federal Employee Program - COVID-19 Service Enhancements
- Capital Blue Cross - COVID-19 Service Enhancements
- CareFirst - COVID-19 Service Enhancements
- CareFirst BlueCross BlueShield - COVID-19 Service Enhancements
- Centene - COVID-19 Service Enhancements
- Cigna - COVID-19 Service Enhancements
- Geisinger Health Plan - COVID-19 Service Enhancements
- Highmark - COVID-19 Service Enhancements
- Horizon Blue Cross Blue Shield of NJ - COVID-19 Service Enhancements
- Humana - COVID-19 Service Enhancements
- Magellan Health - COVID-19 Service Enhancements
- Optima - COVID-19 Service Enhancements
- United Health Care - COVID-19 Telehealth Services
- United Health Care - COVID-19 Physical, Occupational and Speech Therapy Telehealth
- Virginia Premier - COVID-19 Service Enhancements
- State Telehealth Laws and Reimbursement Policies: Spring 2021 Executive Summary: A Comprehensive Scan of 50 States and D.C. Findings & Highlights.
- State Telehealth Laws and Reimbursement Policies: At A Glance Spring 2021
- State Telehealth Laws and Reimbursement Policies: Summary Chart Spring 2021
About Tricare Reimbursement for Telehealth
Specialty Specific Billing and Coding Resources for Clinicians and Practices
- Following are several guidance documents related to billing and coding developed for specific professions/specialty areas as a result of COVID-19:
COVID-19 Claims Reimbursement for Testing and Treatment of the Uninsured
- What is the COVID-19 Claims Reimbursement to Health Care Providers and Facilities for Testing and Treatment of the Uninsured Program? The COVID-19 Claims Reimbursement to Health Care Providers and Facilities for Testing and Treatment of the Uninsured Program provides reimbursements on a rolling basis directly to eligible providers for claims that are attributed to the testing and treatment of COVID-19 for uninsured individuals. The program is authorized via the:
-
- Families First Coronavirus Response Act (P.L. 116-127) and the Paycheck Protection Program and Health Care Enhancement Act (P.L. 116-139), which each appropriated $1 billion to reimburse providers for conducting COVID-19 testing for the uninsured; and the
- CARES Act (P.L. 116-136), which provides $100 billion in relief funds, including to hospitals and other health care providers on the front lines of the COVID-19 response. Within the Provider Relief Fund, a portion of the funding will be used to support healthcare-related expenses attributable to the treatment of uninsured individuals with COVID-19. Funding is provided from the Public Health and Social Services Emergency Fund.
- Who is eligible for funding? Health care providers who have conducted COVID-19 testing of uninsured individuals for COVID-19 or provided treatment to uninsured individuals with a COVID-19 diagnosis on or after February 4, 2020, can request claims reimbursement through the program electronically and will be reimbursed generally at Medicare rates, subject to available funding.
- What services are eligible for reimbursement? Reimbursement will be made for qualifying testing for COVID-19 and treatment services with a primary COVID-19 diagnosis as determined by HRSA (subject to adjustment as may be necessary) , including the following:
- Specimen collection, diagnostic and antibody testing.
- Testing-related visits including in the following settings: office, urgent care or emergency room or via telehealth.
- Treatment, including office visit (including via telehealth), emergency room, inpatient, outpatient/observation, skilled nursing facility, long-term acute care (LTAC), acute inpatient rehab, home health, DME (e.g., oxygen, ventilator), emergency ambulance transportation, non-emergent patient transfers via ambulance, and FDA-approved drugs as they become available for COVID-19 treatment and administered as part of an inpatient stay.
- FDA-approved vaccine, when available.
- For inpatient claims, date of admittance must be on or after February 4, 2020.
View all Frequently Asked Questions about the Program
Provider Relief Fund for Eligible Providers
- $8.5 billion from the American Rescue Plan (ARP) for providers who serve rural Medicaid, Children’s Health Insurance Program (CHIP), or Medicare patients.
- $17 billion for Provider Relief Fund (PRF) Phase 4 payments for a broad range of providers who can document revenue loss and expenses associated with the pandemic.
Scope of Service and BPHC Policies
- Do health centers need to request a change in scope for a provider to deliver in-scope services via telehealth from their home or another site not on Form 5B, assuming all the criteria for doing so (see question above) are met? (Added: 4/7/2020) Health centers do not need to request a change in scope to deliver in-scope services via telehealth on behalf of the health center from the provider’s home or from another location that is not a Form 5B Service Site. In addition, health centers do not need to have "Home Visits" listed on their Form5C: Other Activities/ Locations in order to provide in-scope services via telehealth.
- May health centers provide in-scope services through telehealth to individuals who are not current health center patients? (Added: 3/19/2020) As a result of the Secretary's declaration relating to the current COVID-19 public health emergency, health center providers may deliver in-scope services via telehealth to individuals who have not previously presented for care at a health center site and who are not current patients of the health center for the duration of this public health emergency. This includes triage services, including initial consultations. Telehealth visits are within the scope of project if:
- The individual receives an in-scope required or additional health service;
- The provider documents the service in a patient medical record consistent with applicable standards of practice; and
- The provider is physically located at a health center service site or at some other location on behalf of the health center (e.g., provider’s home, emergency operations center).
Health centers should focus services provided by telehealth on serving patients and other individuals located inside their service area or with areas adjacent to the covered entity’s service area. HRSA recognizes that patients outside these areas may seek health center screenings and triage by telehealth. Health centers that continue to maintain services for target populations in their service area and provide occasional in-scope services via telehealth to individuals outside these areas would be providing services within the Health Center Program scope of project for all such activities. Please review PAL 2020-01: Telehealth and Health Center Scope of Project (PDF – 520 KB) for more information.
- Can a health center use telehealth to provide services to a patient at a location that is not an in-scope service site? Can this occur if neither the health center provider nor the patient is at an in-scope service site (e.g. both the provider and patient are at their respective homes)? (Updated: 4/7/2020) From a Health Center Program scope of project policy perspective, using telehealth to provide services to a patient at a location that is not an in-scope service site is allowable if:
-
-
- The service being provided via telehealth is within the health center's approved scope of project (recorded on Form 5A);
- The clinician delivering the service is a health center provider working on behalf of the health center; and
- The individual receiving the service is a health center patient.
-
HRSA strongly encourages health centers that provide, or are planning to provide, health services via telehealth to consult with professional organizations, regulatory bodies, and private counsel to help assess, develop, and maintain written telehealth policies that are compliant with Health Center Program requirements; federal, state, and local requirements; and applicable standards of practice. HRSA also encourages health centers to consider the range of issues that would support successful implementation of telehealth. Please review PAL 2020-01: Telehealth and Health Center Scope of Project (PDF – 520 KB) for more information.
- How does telehealth impact my 2020 UDS Clinical Measure Reporting? Please refer to this document for guidance.
Federal Tort Claims Act (FTCA)
- Does FTCA coverage extend to telehealth visits with both established patients and non-health center patients? (Updated: 3/27/2020). When in-scope services are provided through telehealth on behalf of a deemed health center to either established patients or individuals who are not patients of the health center, and all other FTCA Program requirements are met, such services are eligible for liability protections under 42 U.S.C. 233(g)-(n), pursuant to 42 CFR 6.6. Health centers and providers are encouraged to consult with private counsel and/or consider the purchase of private malpractice insurance when undertaking activities that may not be within the health center’s scope of project.
- Will HRSA issue a particularized determination for health centers related to COVID-19 activities, similar to the particularized determination that was issued during the H1N1 emergency? (Added: 3/31/2020). HRSA has issued a particularized determination for health center providers (PDF - 35 KB) that clarifies eligibility for FTCA coverage during the COVID-19 pandemic for the provision of grant-supported health services by individuals who have been deemed as Public Health Service employees through the Health Center FTCA Program and the Health Center VHP FTCA Program. It applies to grant-supported health services to prevent, prepare, or respond to COVID-19 (including but not limited to screening, triage, testing, diagnosis, and treatment) to individuals who are established or non-established patients of the health center, whether in person at the health center, offsite (including at offsite programs or events carried out by the health center), or via telehealth.
- During the declared COVID-19 emergency, do FTCA protections apply to health center providers who provide telehealth services to health center patients located across state lines? (Added: 4/8/2020) Health Center FTCA Program regulations at 42 CFR Part 6 provide that coverage applies to “grant-related activities.” Therefore, a key determinant for FTCA coverage is whether the covered entity is providing services within the health center’s scope of project, under the Health Center Program authorizing statute.
PAL 2020-01: Telehealth and Health Center Scope of Project (PDF - 517 KB) highlights some of the relevant considerations for health centers in providing in-scope services through telehealth. Among other things, all providers must comply with applicable state requirements. If they do not—for example, if a provider uses a state license to provide services in a different state where doing so is unlawful under applicable state law—this may jeopardize eligibility for FTCA liability protection. However, some states may have temporarily amended their requirements for providing health care through telehealth to address the needs of the COVID-19 public health emergency.
Health centers that are uncertain of the applicable legal requirements for the provision of health services through telehealth across state lines should consult their private counsel for advice. HRSA cannot provide general assurance of FTCA coverage in all situations, as such determinations are fact-specific. As stated in the FTCA Health Center Policy Manual (PDF - 407 KB), “[w]hen FTCA matters become the subject of litigation, the Department of Justice and the federal courts assume significant roles in certifying or determining whether or not a given activity falls within the scope of employment for purposes of FTCA coverage.”
- Will a deemed health center’s providers remain covered by liability protections under the FTCA if they are directed to provide continuous or permanent services to non-health center inpatients at a local hospital as part of a community-wide emergency response during the declared COVID-19 public health emergency? (Added: 4/16/2020) Continuous or permanent staffing of a hospital or hospital department to provide inpatient care to all hospital patients is not described by the authorizing statute for the Health Center Program, and FTCA coverage generally is not available for such care.
Health centers have discretion to enter into contractual arrangements with hospitals or may allow their providers to enter into arrangements with hospitals to provide hospital-based inpatient care outside the scope of their Health Center Program grants. However, FTCA coverage and other federal benefits directly associated with the Health Center Program would not apply. Providers providing continuous or permanent inpatient care in hospitals through such arrangements may have medical malpractice liability protection through the hospital or another source, and volunteer providers may be eligible for liability protections under federal and state law (including new legal protections for volunteer providers for COVID-19 emergency response via the CARES Act). Health centers should consult with private counsel for legal advice regarding these matters.
Please note that the Health Center FTCA Program regulations and the March 27, 2020, Determination of Coverage for COVID-19-Related Activities by Health Center Providers (PDF - 35 KB) provide for FTCA protection for deemed health centers in the circumstances described in those issuances. The March 27, 2020, Determination of Coverage indicates that health center providers may provide grant-supported health services “to prevent, prepare, or respond to COVID-19 (including but not limited to screening, triage, testing, diagnosis, and treatment)” to individuals who are not patients of the health center, whether at the health center or off-site, and whether in-person or through telehealth. This determination of coverage extends to local COVID-19 community-wide emergency response activities supported by the health center. The Health Center FTCA Program regulations also provide for liability protections for certain described individual emergency situations.
The Health Center Program provides grant support for the delivery of primary and preventive health care service to medically underserved populations and communities. Services provided through the Health Center Program generally consist of outpatient, ambulatory care services for health center patients. As provided for by statute, regulation, and determination of coverage, services may be provided to individuals who are not patients of the health center in limited circumstances.
Medicare and Medicaid Reimbursement
- What policy changes for FQHCs have been instituted as a result of the pandemic? This video will provide an overview of the CMS policy changes for FQHCs:
This Medicare Learning Network Booklet for Federally Qualified Health Centers provides guidance around Telehealth Services Payment, Virtual Communication Services as well as COVID-19 Flexibilities pertaining to payment. Medicare has also issued this more specific guidance document for FQHCs and RHCs: New and Expanded Flexibilities for RHCs and FQHCs During the COVID-19 Public Health Emergency - Revised January 13, 2022. Additionally, CMS has put together this document: COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing. Questions center around a wide variety of topics, but there is a section specific to FQHCs many of the questions relate to telehealth as well as virtual communication services..
- Can health centers bill Medicare for telehealth services as distant site providers? The Coronavirus Aid, Relief, and Economic Security (CARES) Act revises the definition of a distant site in section 1834(m)(2)(A) of the Social Security Act to include FQHCs or RHCs that furnish a telehealth service to an eligible telehealth individual during the COVID-19 public health emergency period. Rural and site limitations are removed, so that telehealth services furnished during the emergency period can be provided regardless of the geographic location of the Medicare beneficiary, including if the patient is at home. In order to be eligible for reimbursement, providers must use telecommunication systems with both audio and video capabilities for two-way, real-time interactive communication.
Distant site telehealth services can be furnished by any health care practitioner working for the RHC or the FQHC within their scope of practice. Practitioners can furnish distant site telehealth services from any location, including their home, during the time that they are working for the RHC or FQHC, and can furnish any telehealth service, including medical outpatient office visits, behavioral health services, and other visits currently eligible under the Medicare telehealth reimbursement policies. To see all services approved for billing as a telehealth service, download the List of Telehealth Services for Calendar Year 2022 (includes both temporary and permanent services)
- Is there current guidance on the reimbursement methodology for distant site telehealth visits under Medicare? See the Medicare guidance document New and Expanded Flexibilities for RHCs and FQHCs During the COVID-19 Public Health Emergency - Revised January 13, 2022.
- Will I be required to get patient consent for telehealth and virtual communication services? Consent is not required for telehealth services. However, beneficiary consent is required for care management and virtual communication services. During the public health emergency (PHE), beneficiary consent may be obtained at the same time the services are initially furnished. For FQHCs, this means that beneficiary consent can be obtained by someone working under general supervision of the FQHC practitioner, and direct supervision is not required to obtain consent. In general, beneficiary consent to receive these services may be obtained by auxiliary personnel under general supervision of the billing practitioner; and the person obtaining consent can be an employee, independent contractor, or leased employee of the billing practitioner. For FQHCs, beneficiary consent to receive these services may be obtained by auxiliary personnel under general supervision of the FQHC practitioner; and the person obtaining consent can be an employee, independent contractor, or leased employee of the FQHC practitioner (see: https://www.cms.gov/files/document/covid-final-ifc.pdf).
- Are there telehealth services where cost sharing has been waived as a result of the pandemic? There are several CPT and HCPCS codes that describe preventive services and should be billed as G2025. When provided by telehealth, cost sharing requirements are waived for these services. .
- What policies have not changed for FQHCs as a result of the pandemic?
- Remote Patient Monitoring (RPM)/Remote Physiologic Monitoring (99453, 99454): CMS clarified toward the end of 2019 that RPM services are not separately billable under Medicare for FQHCs. Since the FQHC Prospective Payment System (PPS) rate includes all services and supplies furnished ‘incident to’ the visit,” CMS feels that RPM costs are already included in the FQHC PPS payment.
-
- eConsult or Interprofessional Consultations (99446-99449, 99451, 99452): CMS guidance says that FQHCs cannot bill for eConsults under Medicare.
- Following is CMS guidance on the New and Expanded Flexibilities for RHCs and FQHCs During the COVID-19 Public Health Emergency - Revised January 13, 2022.
- To see all services approved for billing as a telehealth service: download the List of Telehealth Services for Calendar Year 2022 (includes both temporary and permanent services)
- To receive payment for telephone (audio-only) evaluation and management services (CPT codes 99441, 99442, and 99443) , FQHCs should use HCPCS code G2025. To bill for these services, at least 5 minutes of telephone E/M service by a physician or other qualified health care professional who may report E/M services must be provided to an established patient, parent, or guardian. These services cannot be billed if they originate from a related E/M service provided within the previous 7 days or lead to an E/M service or procedure within the next 24 hours or soonest available appointment.
- To receive payment for online digital evaluation and management services (non-face-to-face, patient-initiated, digital communications using a secure patient portal):
- CPT code 99421 (5-10 minutes over a 7 day period)
- CPT code 99422 (11-20 minutes over a 7 day period)
- CPT code 99423 (21 minutes or more over a 7 day period)
and virtual communication services (HCPCS codes G2012 and G2010), FQHCs must submit an FQHC claim with HCPCS code G0071 (Virtual Communication Services) either alone or with other payable services. For claims submitted with HCPCS code G0071 on or after March 1, 2020, and for the duration of the COVID-19 PHE, payment for HCPCS code G0071 is set at the average of the national non-facility PFS payment rates for these 5 codes. Claims submitted with G0071 on or after March 1 and for the duration of the PHE will be paid at the new rate of $24.76, instead of the CY 2020 rate of $13.53. MACs will automatically reprocess any claims with G0071 for services furnished on or after March 1 that were paid before the claims processing system was updated.
- CaravanHealth put together these two documents that you may find useful:
- Costs for furnishing distant site telehealth services will not be used to determine the FQHC PPS rates but must be reported on the appropriate cost report form. FQHCs must report both originating and distant site telehealth costs on Form CMS-224-14, the Federally Qualified Health Center Cost Report, on line 66 of the Worksheet A, in the section titled “Other FQHC Services”. Since telehealth distant site services are not paid under tthe FQHC PPS, the Medicare Advantage wrap-around payment does not apply to these services. Wrap-around payment for distant site telehealth services will be adjusted by the MA plans.
- NACHC has prepared this Resource Guide on Telehealth Coverage in Medicaid that outlines Medicaid coverage at Health Centers during the pandemic and provides tools for policy changes and recommendations moving forward.
Telehealth Program Development and the Future of Telehealth for FQHCs
- The National Consortium of Telehealth Resource Centers (NCTRC) has a Collection of FQHC Telehealth Resources that is a curation of resources developed by all of the TRCs and designed specifically for FQHCs! This is a great place to start. A few highlights from this collection include:
- Recorded content from the three session FQHC Webinar Series:
- In addition, the Health Center Resource Clearinghouse also has a Collection of COVID-19 Resources for Telehealth.
- Beyond the abundance of materials found in these clearinghouses, here are a few other FQHC specific resources::
-
- We offered a 2-Hour Session on Telehealth in Community Health Centers during our 2019 Telehealth Summit. In this screencast, you will take a closer look at successful established telehealth program models found in FQHCs.
-
- The Center for Care Innovations has put together Telehealth and Telephone Visits in the Time of COVID-19: FQHC Workflows and Guides.
-
- The National School-Based Health Alliance has developed this School-Based Telehealth Playbook for FQHCs as part of a Youth Safety Net Project.
-
- The Health Information Technology, Evaluation, and Quality Center (HITEQ) has put together several useful toolkits and resources, including:
- Getting a New Workflow and Process Started During COVID-19 Pandemic as a quick start guide for health centers (please note that Remote Patient Monitoring billing codes are included in this document - CMS has clarified that RPM services are not separately billable under Medicare for FQHCs. Since the FQHC Prospective Payment System (PPS) rate include all services and supplies furnished ‘incident to’ the visit,” RPM is theoretically already included in the FQHC PPS payment).
- Using Telehealth to Expand PrEP Access in Health Centers. This brief highlights how health centers are using telehealth resources and innovations for HIV Pre-Exposure Prophylaxis (PrEP)
- Electronic Patient Engagement (EPE) Tool Inventory. In the spring of 2020, HITEQ and several PCA and HCCN colleagues developed a survey to gather detailed information on health center experiences with a variety of EPE tools and included questions about product functions, strengths & weaknesses, cost, integration with EHRs, ease of implementation, and quality of vendor support. The results of that survey, as well as interviews and demonstrations are captured in this EPE Tool Inventory.
- The Health Information Technology, Evaluation, and Quality Center (HITEQ) has put together several useful toolkits and resources, including:
-
- The Weitzman Institute provides a series of Project ECHO Clinics on a wide variety of topics geared specifically for FQHCs, many of which include telehealth integrated care models.
-
- The following vendors are offering access to eConsult services for FQHCs during the pandemic. Please note that MATRC is not in a position to either endorse or recommend any of the vendors on this list. We strongly encourage you to do your due diligence when making a vendor selection:
- Free access to Safety Net Connect eConsult Telehealth Portal for primary care physicians
- Free access to ConferMED Coronavirus eConsults for Safety Net Practices
- Free access to The MAVEN Project for eConsults for community health clinics who serve the underserved (The MAVEN Project is available without charge even beyond the pandemic)
- The following vendors are offering access to eConsult services for FQHCs during the pandemic. Please note that MATRC is not in a position to either endorse or recommend any of the vendors on this list. We strongly encourage you to do your due diligence when making a vendor selection:
- How the Rapid Shift to Telehealth Leaves Many Community Health Centers Behind During the COVID-19 Pandemic (Health Affairs)
- Barriers & Challenges to FQHC Use of Telehealth for Substance Use Disorder: A Examination of Policies Affecting FQHCs Pre- and During COVID-19 Emergency (Center for Connected Health Policy)
- Telehealth Practice Among Health Centers During the COVID-19 Pandemic - United States, July 11 - 17, 2020 (CDC)
- Telemedicine Services During COVID-19: Considerations for Medically Underserved Populations (The Journal of Rural Health)
- Community Health Centers COVID-19 Digital Inequities Impacting Access (CaliforniaHealth)
Transitioning from Temporary to Permanent Policies
- The US Health and Human Services has officially renewed the public health emergency (PHE) on multiple occasions, a status that allows many of the waivers and expansions for telehealth that have occurred since the COVID-19 pandemic began in March 2020 to remain active. Each renewal extends the PHE an additional 90 days. The latest renewal, which occurred on April 13, 2022 extends the PHE through July 11, 2022. Key regulatory flexibilities linked to the PHE include the 1135 Waivers, the CMS Interim Final Rule, a number of initiatives under the Families First Coronavirus Response Act and CARES Act legislation, several State Medicaid and CHIP Program flexibilities, HIPAA Enforcement Discretion, Fraud and Abuse Enforcement Discretion and Flexibility Regarding Controlled Substances. Click here for a recent analysis of what policies are linked to the PHE and what are not.
- While the above discusses the status of the federal PHE, many states have already ended their PHE declarations. The Center for Telehealth and eHealth Law (CTeL) has created a 50 State Survey of the status of the PHE for each state. for its members. This is a view of what that survey looks like for July 12. To get ongoing updates, you would need to join CTeL as a member.
- Here is a look at what temporary policy changes might remain post-COVID-19 and what could be issues that policymakers my think merit future action:
- There were some significant changes in telehealth reimbursement as a result of the pandemic and it is likely that the reimbursement, coding and billing policies will eventually revert back to their pre-pandemic guidance. This video provides a really good overview about how telehealth is reimbursed in the U.S., the impact of the public health emergency and some thoughts on how to think about it after the public health emergency:
- This Billing for Telehealth Encounters: An Introductory Guide on Fee-For-Service is a great tool for helping you navigate reimbursement and understand what changes are temporary vs. permanent. Although much of its focus is on fee-for-service Medicare, it also provides information about Medicaid and private payor coverage. In addition, this document also discusses how to bill and code for several types of services that CMS does not consider "telehealth". These include: Remote Communication Technology, Virtual Check-In, Remote Evaluation of Pre-Recorded Patient Information and Interprofessional Internet Consultation.
- To get an even better understanding of Fee for Service Medicare policies, review this document Fee for Service Medicare Telehealth Services and Click Here to see a compilation of questions to CMS related to telehealth reimbursement for FFS Medicare and their responses.
- The Center for Connected Health Policy has been capturing State Medicaid policy related changes (both temporary and permanent) through a webinar series. The Winter and Spring Series webinars were recorded and can be viewed by clicking on the links below.
- Winter 1: Waivers and State Plan Amendments to Address COVID-19
- Winter 2: Provider Engagement & Education During the Public Health Emergency
- Winter 3: Patient Engagement & Education During the Public Health Emergency
- Winter 4: What's Next? A Roadmap for Medicaid Telehealth Policy Beyond the Pandemic
For a written summary of the Winter Series: Telehealth & Medicaid: A Policy Webinar Series - Winter Webinar Series Report
For a written summary of the Spring Series: Medicaid & Telehealth: Summary and Findings from Spring Webinar Series
A Quick Overview of The Flurry of Activities Already Underway to Make Temporary Changes Permanent:- This video provides you with an overview of how telehealth policy is structured in the U.S:
- Here are a number of reports regarding policies and policy recommendations as a result of our experience with COVID-19:
-
- Barriers & Challenges to FQHC Use of Telehealth for Substance Use Disorder: A Examination of Policies Affecting FQHCs Pre- and During COVID-19 Emergency (Center for Connected Health Policy)
- Navigating COVID-19: Health Policy Solutions - Telehealth (Missouri Foundation for Health)
- Removing Regulatory Barriers to Telehealth Before and After COVID-19 (Brookings)
- Telemedicine Services During COVID-19: Considerations for Medically Underserved Populations (The Journal of Rural Health)
- Telehealth & COVID-19 Policy Considerations to Improve Access to Care (UCLA Latino Policy & Politics Initiative/UCLA Health Center for the Study of Latino Health and Culture)
- How the Rapid Shift to Telehealth Leaves Many Community Health Centers Behind During the COVID-19 Pandemic (Health Affairs)
- Taskforce on Telehealth Policy: Findings and Recommendations (NCQA)
- Assessing Legal Responses to COVID-19 (Public Health Law Watch)
- Building a Modern Health Care System: Recommendations from the COVID-19 Federal Policy Work Group (eHealth Initiative)
- Community Health Centers COVID-19 Digital Inequities Impacting Access (CaliforniaHealth)
- Report to Congress: Medicare Payment Policy (MEDPAC)
- The Future of State Telehealth Policy (National Governors Association)
- Medicare and Medicaid: COVID-19 Program Flexibilities and Considerations for Their Continuation (U.S. Government Accountability Office)
- Key Findings from RAND Health Care Research on Telehealth Policy (RAND Corporation)
- Cost Benefit Analysis of Telehealth: March 2020 - September 2020 (CTeL)
- Following are some some of the efforts toward policy changes already under way:
- On Wednesday June 17, the U.S. Senate Committee on Health, Education Labor & Pensions held a hearing on Telehealth: Lessons from the COVID-19 Pandemic. Our own Karen S. Rheuban joined Joseph C. Kvedar, Sanjeev Arora and Andrea Willis to share testimony, contributing to the discussion about what temporary telehealth changes should be made permanent in federal and state policies. Watch Here!
-
- On June 29th, 340 organizations signed a letter urging Congressional leaders to make telehealth flexibilities created during COVID-19 pandemic permanent. Read the Letter Here!
-
- The Taskforce on Telehealth Policy had invited public input as it develops policy recommendations for advancing quality and patient experience while establishing a stable, long-term environment that fosters the growth and integration of remote services within the healthcare system. Learn more here.
-
- The American Hospital Association has written an open letter addressed to President Trump regarding the need to do to enable more for hospitals and health systems to provide virtual care.
-
- The Medicare Payment Advisory Commission (MEDPAC) presented policy options for expanding telehealth in Medicare. See the presentation here.
-
- In mid-November, the US Department of Veterans Affairs released an interim final rule allowing VA health care professionals to practice across state lines beyond the COVID-19 public health emergency as long as it is in accordance with the scope and requirements of their VA employment, regardless of state licensing requirements. Read the full interim final rule here.
-
- CMS finalized its CY2021 Physician Fee Schedule and issued this fact sheet The 2021 PFS makes permanent a number of codes that are currently on the Medicare telehealth list as a result of the COVID-19 public health emergency (PHE) and adds others provisionally through the end of the year in which the PHE ends. CMS also addresses a number of other issues, such as frequency limits for nursing facility visits furnished via telehealth. Clarification is given around issues such as the ability of physical, occupational and speech language pathologists to furnish brief online assessment and management services and certain requirements related to remote physiologic monitoring. CMS also specifies that the telehealth restrictions do not apply when a beneficiary and practitioner are in the same location even if conducted via audio/video technology. In the absence of the COVID-19 PHE declaration, CMS will not continue to recognize audio-only codes that were added in 2020 in response to the COVID-19 PHE. However, based on comments received, they are establishing a new HCPCS G-code describing 11-20 minutes of medical discussion to determine the necessity of an in-person visit.
- The Center for Connected Health Policy has also developed this Fact Sheet specific to the telehealth related provisions.
- CMS finalized its CY2021 Physician Fee Schedule and issued this fact sheet The 2021 PFS makes permanent a number of codes that are currently on the Medicare telehealth list as a result of the COVID-19 public health emergency (PHE) and adds others provisionally through the end of the year in which the PHE ends. CMS also addresses a number of other issues, such as frequency limits for nursing facility visits furnished via telehealth. Clarification is given around issues such as the ability of physical, occupational and speech language pathologists to furnish brief online assessment and management services and certain requirements related to remote physiologic monitoring. CMS also specifies that the telehealth restrictions do not apply when a beneficiary and practitioner are in the same location even if conducted via audio/video technology. In the absence of the COVID-19 PHE declaration, CMS will not continue to recognize audio-only codes that were added in 2020 in response to the COVID-19 PHE. However, based on comments received, they are establishing a new HCPCS G-code describing 11-20 minutes of medical discussion to determine the necessity of an in-person visit.
-
- US Rep. Ann Wagner (R-MO) introduced HR 7992 (Telehealth Act) that combines nine telehealth bills into one piece of legislation. The legislation would provide various expansions in Medicare reimbursement for telehealth, including coverage for telemental health services without geographic and site restrictions, allowing FQHCs and RHCs to be distant site providers and more. The nine federal bills include:
- HR 7338: The Advancing Telehealth Beyond COVID-19 Act
- HR 5473: The EASE Behavioral Health Services Act
- S 4039: The Telemedicine Everywhere Lifting Everyone’s Healthcare Experience and Long-Term Health (TELEHEALTH) HSA Act
- HR 3228: The VA Mission Telehealth Clarification Act
- HR 4900: The Telehealth Across State Lines Act
- S 4103: The Telehealth Response for E-prescribing Addiction Therapy Services (TREATS) Act
- HR 7233: The KEEP Telehealth Options Act
- S 3988: The Enhancing Preparedness Through Telehealth Act
- HR 7187: The HEALTH Act
- US Rep. Ann Wagner (R-MO) introduced HR 7992 (Telehealth Act) that combines nine telehealth bills into one piece of legislation. The legislation would provide various expansions in Medicare reimbursement for telehealth, including coverage for telemental health services without geographic and site restrictions, allowing FQHCs and RHCs to be distant site providers and more. The nine federal bills include:
-
- Senator Schatz (S 1512) has introduced the Connect Act for Health - 2021 - this video provides an overview of the key provisions (of which there are many):
-
- CMS has proposed its CY2022 Physician Fee Schedule and issued this fact sheet CMS is soliciting public comments before the policies will be finalized later this year. Public comments are due no later than 5 PM on September 13, 2021. The Center for Connected Health Policy has developed this Fact Sheet specific to the telehealth related provisions.
- If you want a snapshot of telehealth policies for all States, take a look at the following documents:
- For a deeper dive on all State Telehealth reimbursement and reimbursement related policies, visit: https://www.cchpca.org/all-telehealth-policies/
- You may be interested in reading this paper on State Medicaid Medical Directors Network:: Perspectives on Telehealth Modernization
Telehealth Quality and Performance Improvement
- Many federal and state policies were loosened in response to this public health emergency. This has enabled some "sloppy" telehealth care. Start thinking now about changes you will need to make to fix "sloppy" and to ensure you have the right infrastructure and tools in place to meet legal, regulatory and clinical standards of care for your patients/clients. In addition to all of the Best Practices found in this toolkit, here are a few toolks that can help you think about the bigger picture:
- The American Medical Association has put together a really nice Telehealth Implementation Playbook that would be useful once you have the ability to step back from the immediate need to get up and running and to think more strategically for longer term planning.
- The Medical University of South Carolina (MUSC) has put together this Telehealth Service Implementation Model (TSIM): A Framework for Telehealth Service Development, Implementation and Sustainability.
- The California TRC has developed this comprehensive Telehealth Program Developer Kit: A Roadmap for Successful Telehealth Program Development: as well as this Compendium of Best Practices in Telehealth Services.
- The American Academy of Family Physicians has developed A Toolkit for Building and Growing a Sustainable Telehealth Program in Your Practice.
- For those working with rural communities, the Rural Health Information Hub has developed a Rural Telehealth Toolkit
- Don't expect "business as usual". Prepare for a tsunami of patients who have delayed care and will need it. Prepare also for patients who will continue to delay care because they are fearful of exposure by coming into your office or a health care facility. Start thinking NOW about how to use the telehealth tools you have started putting into place to address this oncoming wave. Start thinking now also about quality of care. Here are a few resources to serve as food for thought:
- We have now let the genie out of the bottle and hundreds of thousands of providers and patients will have experienced telehealth for the first time. Some will recognize its value and want to continue. What data should you be collecting now so you can both demonstrate telehealth quality, assess performance improvement and be prepared to make a case for policy changes if/when needed?
- Here is an attempt at a first draft of a COVID-19 Measure Framework developed by SPROUT. It is still a work in progress, but should provide some food for thought.
- CaravanHealth has developed this Guidance on Collecting Clinical Quality Measures in a Virtual Visit
- CMS has issued this Telehealth Guidance for Electronic Clinical Quality Measures (eCQMs) for Eligible Professional/Eligible Clinician 2021 Quality Reporting. There are 39 telehealth-eligible eCQMs for the 2021 performance period. This guidance applies to the following programs:
- Quality Payment Program: The Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (Advanced APMs)
- APM: Comprehensive Primary Care Plus (CPC+)
- APM: Primary Care First (PCF)
- Medicaid Promoting Interoperability Program for Eligible Professionals
- For those wanting to assess implementation, workflows, etc...as these are being together, the Consolidated Framework for Implementation Research is a great place to start.
- We have some preliminary data reports coming out regarding trends and impact on telehealth from COVID-19. Here are several recent ones:
- As the Country Reopens Safety Concerns Rise (Sage Growth/Blackbook Research) does a good job capturing where we are right now
- The Impact of COVID-19 Pandemic on Outpatient Visits: Changing Patterns of Care in the Newest COVID-19 Hot Spots (Commonwealth Fund)
- The Impact of the COVID-19 Pandemic on Outpatient Care: Visits Return to Pre-pandemic Levels, but Not for All Providers and Patients (Commonwealth Fund)
- Medicare Beneficiary Use of Telehealth Visits: Early Data from the Start of the COVID-19 Pandemic (ASPE)
- Monthly Telehealth Regional Tracker (FAIR Health)
- Special Report: The Rapid Transition to Telemedicine Insights and Early Trends (Press Ganey)
- Telehealth Use Among Older Adults Before and During COVID-19 (National Poll on Healthy Aging - University of Michigan)
- Services Delivered via Telehealth Among Medicaid & CHIP Beneficiaries During COVID-19: Preliminary Medicaid & CHIP Data Snapshot for Services through June 30, 2020 (CMS)
- Trends in the Use of Telehealth During the Emergence of the COVID-19 Pandemic - United States, January - March 2020 (CDC)
- COVID-19 Telehealth Impact Study (The COVID-19 Healthcare Coalition Telehealth Impact Study Work Group)
- The Future of Telehealth in School-Based Health Centers: Lessons from COVID-19 (Journal of Pediatric Health Care)
- In-Person and Telehealth Ambulatory Contacts and Costs in a Large US Insured Cohort Before and During the COVID-19 Pandemic (JAMA Network)
- Medicare and Telehealth: Coverage and Use During the COVID-19 Pandemic and Options for the Future (Kaiser Family Foundation)
- Patient Characteristics Associated with the Successful Transition to Virtual Care: Lessons Learned from the First Million Patients ( Mass General Hospital)


